Introduction
Gingivitis and periodontal disease were the second most common diseases in Korea in 2018 and have been ranked as the most common diseases since 2019. The annual number of patients with gingivitis and periodontal disease reached 16 million in 2020 and increased to 17.4 million in 2021 [1]. Periodontal disease is related to bacteria, systemic diseases, demographic factors, health behaviors, genetic factors, psychological factors, dietary habits, and oral health behaviors [2].
Among these factors, smoking is the leading cause of disease burden, along with hypertension and alcohol consumption [3]. Moreover, oral cancer and periodontal disease are closely related to smoking [4-6]. Smokers have 2.4- and 4.5-fold increased risks of tooth loss and edentulism compared to non-smokers [7] and may experience nutritional deficiencies due to tooth loss, suggesting that smoking is closely related to periodontal disease [8]. As the risk of smoking has become known worldwide, awareness of smoking has changed. Efforts around the world are underway to establish policies, systems, and social atmospheres that discourage smoking [9].
Periodontal diseases can be managed through continuous dental plaque management [10] and prevented through professional and self-management [11,12] using antibiotics [13], mouthwash [14], and physical methods such as brushing [11].
Oil pulling is a traditional Ayurvedic treatment practiced in ancient India to maintain oral health. It is effective in treating more than 30 systemic diseases, including diabetes and asthma, and can be easily and economically performed. Hence, oil pulling has been extensively used worldwide for decades [15]. Traditionally, sesame oil has been used, although other types of oils such as coconut oil and sunflower oil are now recommended [16]. Oil pulling involves swishing the oral cavity with oil and is most effective when conducted in the morning on an empty stomach. For adults, approximately 10 ml of oil is generally used [15]. Coconut comprises >92% medium-chain triglycerides, about 50% of which are lauric acid, which has antibacterial and anti-inflammatory effects [17]. Hence, oil pulling using coconut oil has been used as additional chemotherapy for mechanical oral hygiene [18]. Additionally, oil pulling has effects like those of detergents [8] and is effective for removing harmful heavy metals from saliva [9], managing systemic and chronic diseases [8], and reducing plaque formation [19], dental caries [19], and bad breath odor [20].
Most studies on smoking and periodontal conducted are secondary analyses of big data such as the National Health and Nutrition Examination Survey, with only a few studies directly applying clinical interventions. Furthermore, few studies have investigated the effects of coconut oil as a clinical intervention for periodontal disease. Thus, although oil pulling using coconut oil is a practical intervention for the management of periodontal health in smokers, research evidence is insufficient and there is a need for systemic measures to reduce and manage periodontal disease. Therefore, this study evaluated the effects of a 4-week coconut oil pulling intervention on periodontal health management in smokers.
Methods
1. Research participants
This study included 30 smokers who visited a dental medical institution in G region between August 5 and October 20, 2022. The total sample size was based on the number of participants required for repeated-measures analysis of variation (ANOVA) with an effect size of 0.25, significance level of 0.05, power of 0.8, two groups, and three measurements. The required sample size was 28; however, considering a dropout rate of approximately 10%, 30 participants were enrolled. This study was approved by the Institutional Review Board (IRB) for ethical considerations (IRB No. 1041465-202208-HR-001-23). The participants were enrolled only after receiving detailed explanations of the study content and purpose and providing written consent.
2. Research methods
A total of 15 participants were assigned to each of the control and experimental groups. The control group received sterilized distilled water (JW Life Science Co., Ltd., Korea), aliquoted in three bottles with volumes of 1,000 ml and 200 ml. The experimental group received 500 ml of organic coconut oil (Honest Organic Coconut Oil HONEST SUPPERFOOD, EARTH BORN CO., LTD., Thailand; certified by Konkuk ECO Certification Agency; Certification number: 50-8-104). Both groups were instructed to wash their teeth with 5-10 ml of the respective intervention solution for 2-3 minutes after brushing every morning for four weeks. Compliance with the instructions was confirmed by text messages. The clinical indicators were evaluated three times for teeth #16, #11, #26, #36, #31, and #46 (baseline, after 4 weeks, after 8 weeks). Oral dryness and patient quality of life were subjectively evaluated twice (at baseline and after 8 weeks).
3. Research tool
Periodontal pocket depth >4 mm and sites of Bleeding on Probing (BOP) were recorded and summed for analysis. The Patient Hygiene Performance index (PHP index) was evaluated as follows. The dental plaque attachment pattern was evaluated by applying a disclosing solution and washing twice. Areas with and without staining by the disclosing solution were scored 1 and 0 points, respectively. Each tooth was divided into five parts according to the mesial, distal, and medial (incisal, central, and cervical margins) surfaces, with maximum and minimum scores of 5 and 0 points, respectively.
Oral dryness was evaluated using a six-item visual analog scale from 0 points for ‘no oral dryness’ to 10 points for ‘severe oral dryness’. A higher score indicated greater oral dryness severity. Oral health-related quality of life was evaluated using the Oral Health Impact Profile (OHIP-14) rated on a scale from five points for ‘not at all’ to one point for ‘very often’. A higher score indicated a greater oral health-related quality of life.
4. Data analysis
The data collected in this study were analyzed using IBM SPSS program (ver 21.0; IBM Corp., Armonk, NY, USA) with two-tailed tests at a significance level of 0.05. Participant homogeneity was assessed by χ2 and independent sample t-tests as normality was satisfied for sex, age, number of missing teeth, and number of cigarettes smoked per day. The hypothesis was tested as follows for the experimental and control groups. As the dependent variables (BOP, pocket depth, PHP index) satisfied the conditions of parametric tests, two-way repeated measure ANOVA was conducted to identify the interaction effects of group and time. Mauchly’s sphericity test was conducted to confirm the homogeneity of variance. As both oral dryness and quality of life satisfied normality, paired and independent t-tests were conducted with reliabilities of 0.897 and 0.954, respectively.
Results
1. Homogeneity test of participant characteristics
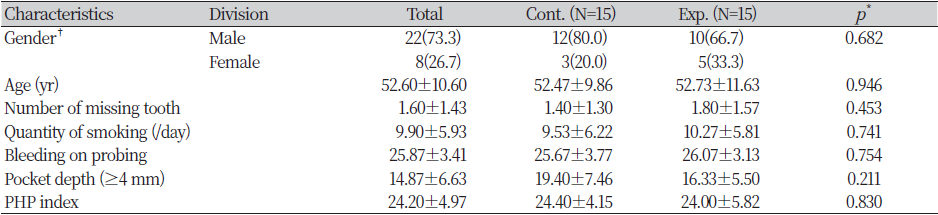
The characteristics (sex, age, number of missing teeth, number of cigarettes smoked per day) and baseline BOP, pocket depth, and PHP index were similar between the control and experimental groups (p>0.05) <Table 1>.
2. Changes in clinical indicators of periodontal disease following the coconut oil intervention
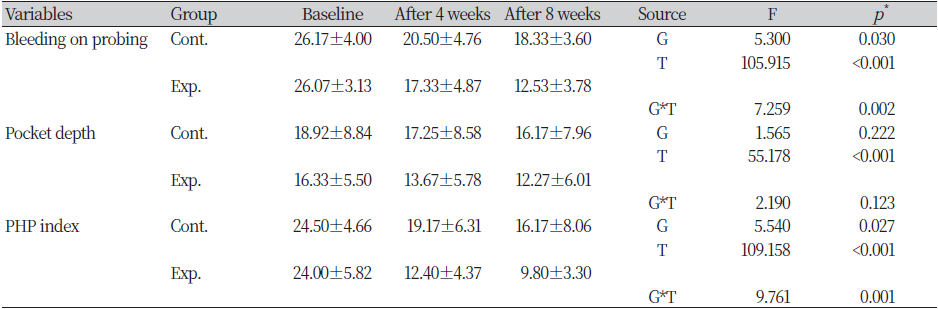
<Table 2> shows changes in the clinical indicators of periodontal disease following the coconut oil intervention. The BOP changed from 26.17 to 18.33 in the control group and from 26.07 to 12.53 in the experimental group, with significant differences by group (p=0.030) and time (p<0.001). Similarly, the interaction effects differed significantly (p=0.002). Pocket depth decreased from 18.92 to 16.17 in the control group and from 24.50 to 16.17 in the experimental group the differences by group were not significant (p=0.222); however, the differences were significant by time (p<0.001). The interaction effects did not differ significantly (p=0.123). The PHP index decreased from 24.50 to 16.17 in the control group and from 24.00 to 9.80 in the experimental group, with significant differences by group (p=0.027) and time (p<0.001). Significant differences in interaction effects were also observed (p=0.001).
3. Changes in oral dryness and oral health-related quality of life following the coconut oil intervention
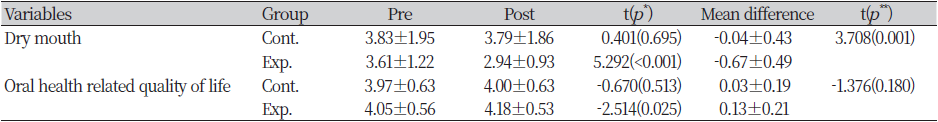
<Table 3> shows changes in oral dryness and oral health-related quality of life following the coconut oil intervention. Oral dryness decreased significantly in the experimental group after the intervention (p<0.001) and compared to the control group (p=0.001). The oral health-related quality of life increased in the experimental group after the coconut oil-pulling intervention (p=0.025); however, compared to the control group, the difference was not significant (p=0.180).
Discussion
Periodontal disease is a chronic inflammatory condition related to various factors such as smoking, chronic diseases, dietary habits, and personal hygiene management. Among these risk factors, smoking has the greatest effects on periodontal disease [21,22]. Smoking constricts blood vessels and affects fibroblasts in connective tissues, thereby delaying periodontal tissue recovery [21]. Therefore, this study investigated the improvement of periodontal health following a coconut oil-pulling intervention in smokers with chronic periodontal disease.
Our findings showed a significant decrease in BOP in the experimental group that received coconut oil intervention compared to the control group (p=0.030), with a significant group-by-time interaction effect (p=0.002). This finding was consistent with those reported by Lee et al. [23], who used coconut oil to treat patients with gingivitis. Other studies also reported significant BOP reduction in coconut oil intervention groups compared to the chlorhexidine intervention group, with significant interaction effects between groups and over time [24,25]. As demonstrated in the present and previous studies, coconut oil is as effective as chlorhexidine in reducing bad breath and microorganisms [20]. Coconut oil not only decreases dental plaque formation but also has effects as an adjunctive therapy for the treatment of gingivitis [17]. Thus, coconut oil may effectively reduce gingival bleeding in smokers.
Like BOP, the coconut oil intervention group showed a significantly reduced PHP index compared to that in the control group (p=0.027), with a significant group-by-time interaction effect (p=0.001). Consistent with our findings, Sood et al. [20] reported a significant decrease in PHP index in the experimental group treated with coconut oil. Our findings revealed that BOP and PHP index had significant interaction effects between groups and over time, consistent with previous studies reporting continuous decreases in BOP and PHP index over time [26].
A previous study [24] reported that chlorhexidine, which is commonly used in clinical practice, caused oral discoloration. To replace chlorhexidine, coconut oil pulling was recommended as an evidence-based intervention for patients receiving implant placement, in which pulling was expected to contribute to reduced dental expenses and periodontal health management due to its safety without a dentist’s prescription. Based on this evidence, the active recommendation of coconut oil pulling to smokers can benefit periodontal health management in smokers.
Oral dryness and oral health-related quality of life evaluated using OHIP-14 were improved in the coconut oil-pulling intervention group, an intervention that can be easily and repeatedly applied in daily life. Lim et al. [27] reported that oral care interventions such as oral exercise, brushing, and denture management improved oral dryness and oral health-related quality of life in denture wearers. Like brushing, flossing, interdental products, and regular dental care, which improved oral health by 4.0-22.0% [28], oral rinsing solution using coconut oil also effectively improved oral health.
Smokers experience more infections by pathogens that cause periodontal disease and have a 1.85-fold higher risk of periodontal disease compared to non-smokers [29]. To prevent the progression of periodontal disease in smokers, coconut oil pulling was performed for 4 weeks in the present study. Our results showed improvement in all measurement variables, including BOP, PHP index, oral dryness, and oral health-related quality of life. This objective evidence suggests that coconut oil pulling can be a simple and effective intervention to improve periodontal health in smokers. Therefore, coconut oil pulling is expected to be used in clinical practice as a useful intervention for smokers.
However, this study has several limitations. As participant compliance with instructions for daily coconut oil oral rinsing was confirmed through text messages, objective and accurate assessment was limited. In addition, coconut oil pulling was not conducted on an empty stomach, as recommended in other studies for maximum effect.
Additional studies are needed to address these limitations, with improved study design to verify the effects of oil pulling. Moreover, retrospective studies with long-term follow-ups are needed to provide meaningful findings.
Conclusions
This study assessed the improvement in periodontal health after a coconut oil-pulling intervention in smokers with chronic periodontal disease. The results were as follows:
1. BOP changed from 26.17 to 18.33 in the control group and from 26.07 to 12.53 in the experimental group. There were significant differences by group (p=0.030) and time (p<0.001). Similarly, there were significant differences in the interaction effects (p=0.002).
2. PHP index decreased from 24.50 to 16.17 in the control group and from 24.00 to 9.80 in the experimental group. There were significant differences by group (p=0.027) and time (p<0.001). There were also significant differences in the interaction effects (p=0.001).
3. Oral dryness decreased significantly in the experimental group after the coconut oil-pulling intervention (p<0.001) and compared to the control group (p=0.001). The oral health-related quality of life increased in the experimental group after the coconut oil-pulling intervention (p=0.025); however, compared to the control group, the oral health-related quality of did not differ significantly (p=0.180).
These findings demonstrated that coconut oil pulling significantly decreased BOP and PHP index in smokers while improving oral dryness, suggesting that it may be a valuable and effective intervention for the management of periodontal health in smokers. Follow-up studies are needed to address the limitations of this study and verify the effects of coconut oil pulling to develop systematic programs to improve periodontal health in smokers.