Introduction
The oral cavity maintains its functions—including mastication, deglutition, and pronunciation—via interactions among teeth, nearby tissues, and muscles of the mouth. Mastication and deglutition are the first processes of digestion where the interaction among teeth, masticatory muscles, and tongue muscles allows for mixing food with saliva, forming a bolus, and moving it to the esophagus [1]. Tooth loss decreases oral muscle mass and, consequently, reduced muscle strength can diminish the efficiency of mastication and deglutition [2].
The average teeth number in different age groups of Korean populations is 25.3 for 50-59-year-olds, 22.5 for 60-69-year-olds, and 15.4 for ≥70-year-olds. Tooth loss worsens with increasing age, and, especially in people ≥70 years old, the number of remaining teeth has been reported to be drastically reduced [3, 4]. Tooth loss and use of dentures cause limitations in food selection, and due to difficulties in forming adequate-sized food bolus, these individuals selectively consume soft food, which hinders with activation of oral muscles, such as masticatory muscle [5]. Moreover, selective food consumption results in reduced consumption of essential nutrients, reduced total energy intake, and nutritional imbalance that consequently causes negative effects on health and muscle maintenance in the elderly population [6].
33.7% of the elderly population experiences dysphagia due to reduced muscle tension and delayed muscle spasm [7]. This results not only in difficulties with food consumption but also other complications—such as aspiration pneumonia, malnutrition, and dehydration—that are often caused by difficulties in medication intake and food entering trachea. In severe cases, these complications can lead to mortality [8,9], Furthermore, 19.7% of the elderly population experiences pronunciation problems that is around 20-fold greater than the 1.1% of the 20-39 years old population [10]. Tongue muscles that play an important role in deglutition and pronunciation are crucial in the deglutition process of swallowing bolus, on top of their supplementary action for mastication [11]. Reduced lip muscle strength causes food to spill out of the mouth and the inability to move food to the occlusal surface, further leading to avoidance of social activities involving meals and overall negative influence in oral health-related quality of life [12].
Oral function is crucial not only for recognition of food intake and supplying nutrition but also for sensory stimulation that brings joy from consuming quality food. A recent study has suggested that oral myofunction during mastication stimulates the brain cortex by increasing the cerebral blood flow by 40% as well as brain activity and cognitive function, consequently preventing dementia [13]. In addition, the elderly population with poorer oral health has an increased risk for brain-related diseases (e.g. cerebrovascular disease and Parkinson’s disease) as well as other diseases (e.g. amyotrophic sclerosis) and exhibit more rapid aging. These findings suggest that reduced oral function is a risk factor of reduced cognitive function [14-16], and appropriate oral stimulation can assist with the prevention of dementia [17].
Around 15-20% of the world population are elderly, and dental diseases (9.7%) and dementia (9.9%) are two of the top 5 most common future diseases in the elderly population [18]. With aging, cognitive function worsens, and, thus, dementia has become a hot topic in the elderly community. Cognitive function plays a crucial role in daily activities and is closely associated with deteriorating health; maintenance of oral health until elderly age is an intervention to improve nutritional intake via mastication and deglutition and cognitive function among various oral functions [19,20].
Although previous studies have assessed associations among tooth loss, masticatory function, and cognitive function, there are few studies that have assessed oral myofunction and the related oral environment or cognitive function. In this study, we assessed the correlation between oral myofunction and oral environment in a group of elderly participants with mild cognitive impairment and a normal control group, to emphasize the importance of oral health for maintenance of health in elderly population and the need for oral health and myofunction maintenance. In addition, we aim to provide these findings as foundational data for the development of elderly oral health improvement programs.
Methods
1. Subjects
This study was approved by the research ethics board of K University (KYU-2018-143-01). This study was performed on a cohort of elderly (≥65 years old) subjects from a senior nursing home daycare center in the city (N) and a senior center at an apartment in the city (D), after explaining them of the study purpose and ethical aspects of the study and obtaining their consent. The subjects were categorized into a group of elderly subjects with mild cognitive impairment visiting the day care center and a group of normal elderly subjects visiting the senior center at an apartment. For oral examination, both dentulous and edentulous subjects were included. The subjects who did not understand the examination process or who refused to further participate in the study during the examination were excluded from the study. The calculated sample size using G-power program 3.1.9.2 version with the effect size of 0.15, a significance level of 0.05, power of 0.80, and the number of predictors 4 was 55. Overall, 60 subjects were included in the final cohort for analysis.
2. Methods
Oral myofunction was assessed via measurement of tongue muscle and lip muscle strengths by the investigator. Tongue muscle was assessed using IOPIR (IOPI Medical, Redmond, WA, USA), where the tongue valve was connected to the equipment and the maximum pressure of the tongue when pressured with the palate was measured. Lip muscle was assessed using Lip de CumR (Cosmo Instruments Co., Ltd., Tokyo, Japan). Plastic lip holder connected to a sensor was placed on the lips, and a measurement was made after instructing the subject to exert maximum pressure in the perpendicular direction for 3 seconds. All outcomes were an average of 3 independent measurements.
Assessment of oral environment was performed by a dentist and two investigators, based on the Korea National Health and Nutrition Examination Survey (KNHANES) guidelines. In detail, oral examination outcomes, use of dentures, and the need for periodontal treatment were assessed. Implant teeth were counted as functional teeth, and the numbers of natural teeth and functional teeth were separately recorded.
3. Data analysis
Data analysis was performed using PASW Statistics version 18.0 (IBM Co., Armonk, NY, USA) software. The subjects’ general characteristics, oral myofunction, and oral environment were described with descriptive statistics. In addition, oral myofunction, cognitive function, and group-specific oral environment were compared with t-tests, and correlations between each of the variables were assessed using Pearson’s correlation. P values of less than 0.05 were considered statistically significant.
Results
1. General characteristics and oral environment based on cognitive impairment status
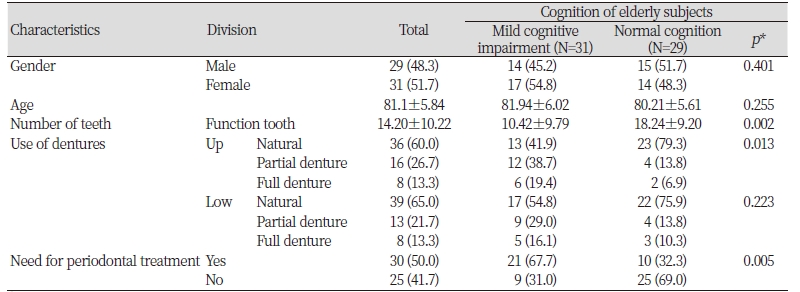
Overall, there were 31 elderly subjects with mild cognitive impairment and 29 normal elderly subjects. There were 29 males and 31 females in the final cohort (p>0.05). The mean age of the cohort was 81.1 years, ranging between 67 and 93 years. There was no significant difference in age between the different groups (p>0.05). For the number of remaining teeth in each group, the number of functional teeth was greater in the normal elderly subjects (18.24±9.20) compared to the elderly subjects with mild cognitive impairment (10.42±9.79, p<0.05). Furthermore, the number of natural teeth was also greater in normal elderly subjects (11.31±8.23) compared to the elderly subjects with mild cognitive impairment (6.13±8.06, p<0.05). Denture use was more common in the elderly subjects with mild cognitive impairment compared to the normal elderly subjects, and there was a significant difference in the use of maxillary dentures between the two groups (p<0.05).
The need for periodontal treatment was greater in the elderly subjects with mild cognitive impairment (67.7%) compared to the normal elderly subjects (32.3%, p<0.05) <Table 1>.
2. General characteristics of oral myofunction
For gender-specific oral myofunction, tongue muscle strength was greater in males (38.39±8.86) than females (35.14±7.63, p>0.05). Similarly, lip muscle strength was also greater in males (9.57±3.68) compared to females (9.19±2.60, p>0.05).
For oral myofunction according to age, both tongue muscle and lip muscle strengths were greater in the group of <81 years old elderly subjects (38.99±8.51;10.44±3.50) compared to the group of ≥81 years old elderly subjects (34.85±7.84, p>0.05 ; 8.50±2.56, p<0.05).
For oral myofunction according to the number of functional teeth, both tongue muscle and lip muscle strengths were greater in the group with ≥15 functional teeth (40.91±7.3; 10.54±3.40) compared to the group with <15 functional teeth (32.52±7.14, p<0.001; 8.20±2.41, p<0.05).
Lastly, for oral myofunction according to denture use, tongue muscle strength of subjects without maxillary denture (40.51±7.46) was greater than that of subjects using full dentures (30.40±5.49, p<0.001), while the subjects without mandibular denture had greater tongue muscle strength (39.92±7.33) compared to the subjects using full dentures (31.50±5.41, p<0.001). Lip muscle strength of the subjects without maxillary dentures (10.39±3.63) was greater than that for the subjects using full dentures (8.12±1.05, p<0.05) <Table 2>.
|
Table 2. Oral myofunction according to general characteristics (N=60) 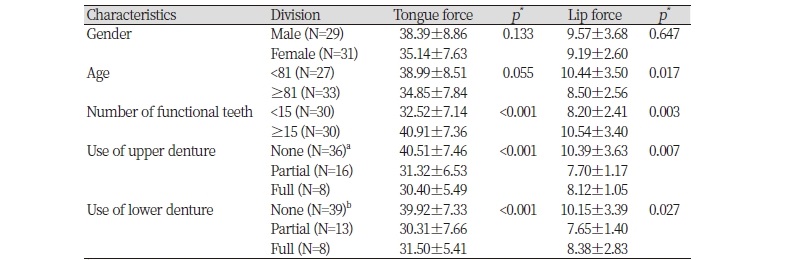
|
|
|
*by t-test, ANOVA(Scheffe Test) a,bThe same characters are not significant by Scheffe multiple comparison (p<0.001, p<0.05). |
|
3. Oral myofunction and oral environment based on cognitive impairment status
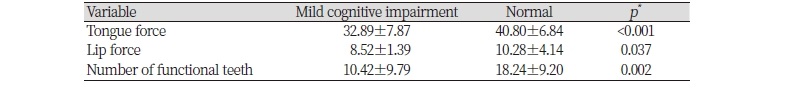
Both tongue muscle and lip muscle strengths of the subjects with mild cognitive impairment (32.89±7.87; 8.52±1.39) were weaker compared to the normal elderly subjects (40.80±6.84, p<0.001; 10.28±4.14, p<0.05). Furthermore, the number of functional teeth was also lower in the subjects with mild cognitive impairment (10.42±9.79) compared to the normal elderly subjects (18.24±9.20, p<0.05) <Table 3>.
4. Correlation analysis among oral myofunction, oral environment, and cognitive function
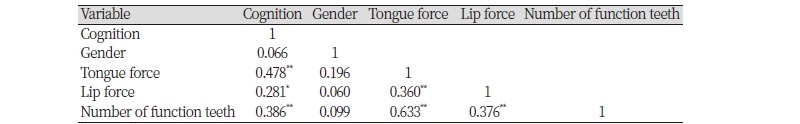
Correlation analyses among oral myofunction, oral environment, and cognitive function have demonstrated significant positive correlations between cognitive function and tongue muscle strength (r=0.478, p<0.001), lip muscle strength (r=0.281, p<0.05), and the number of functional teeth (r=0.386, p<0.001). In addition, tongue muscle strength had a significant positive correlation with lip muscle strength (r=0.360, p<0.001) and the number of functional teeth (r=0.633, p<0.001). Lastly, there was a significant positive correlation between lip muscle strength and the number of functional teeth (r=0.376, p<0.001) <Table 4>.
Discussion
To assess the correlations among oral myofunction, oral environment, and cognitive function, we assessed a group of elderly subjects with mild cognitive impairment and a group of normal elderly subjects. The normal elderly subjects had about 8 more functional teeth compared to the elderly subjects with mild cognitive impairment, and the number of natural teeth was also greater in the normal elderly subjects. A previous prospective study by Yamamoto et al. [21] reported that subjects with very few natural teeth and no dentures exhibited a significantly higher risk of dementia compared to subjects with normal dentition (≥20 teeth). This finding suggests that maintenance of health dentition and masticatory function has an important effect on cognitive function [22], further emphasizing the need for oral maintenance to prevent tooth loss.
Among oral myofunction according to the age group, both tongue muscle and lip muscle strengths were significantly greater in the subjects who are <81 years old (38.99±8.51; 10.44±3.50) compared to the subjects who are ≥81 years old (34.85±7.84; 8.50±2.56). Aging leads to denaturation and loss of muscles, consequently weakening body functions. Progressive weakening of muscles is also observed in oral muscles leading to reduced oral myofunction responsible for mastication, deglutition, and pronunciation [23]. These findings suggest the association between systemic muscle strength and oral muscle strength, and both systemic and oral muscle exercises are required to prevent oral muscle loss from aging.
For oral myofunction according to the number of functional teeth, the group with ≥15 remaining functional teeth exhibited greater tongue and lip muscle strengths compared to the group with <15 remaining functional teeth. In addition, tongue muscle strength was greater in the subjects without dentures compared to the subjects using full dentures. These observations imply that tooth loss can lead to deterioration of oral muscle and reduced masticatory function. Nonetheless, individuals with a high number of remaining teeth can maintain their masticatory function despite aging [24], suggesting that aging itself is not a risk factor of disabilities in oral myofunction aside from mastication. Tooth loss results in reduced masticatory function, forcing selective consumption of small and soft food. This further hinders activation of masticatory muscles, consequently leading to reduced oral myofunction [25]. Therefore, masticatory function is not largely affected in elderly individuals with healthy dentition, and prosthetic treatment to recover teeth function was important in cases of tooth loss [26].
The need for periodontal treatment was greater in the subjects with mild cognitive impairment (67.7%) compared to the normal elderly subjects (32.3%), highlighting the importance of management in vulnerable populations. The components of the masticatory system—including teeth, periodontal ligament, and alveolar bone—should be maintained in a healthy condition through regular oral examination. Furthermore, diseases that have direct impacts on mastication and deglutition—such as dental caries, periodontal diseases, and malocclusion—require early treatment [27].
Both tongue and lip muscle strengths of the elderly subjects with mild cognitive impairment were weaker compared to the normal elderly subjects. Similarly, the number of functional teeth was fewer in the elderly subjects with mild cognitive impairment. These findings can be explained by the outcomes of the correlation analyses that showed significant positive correlations between cognitive function and tongue muscle strength, lip muscle strength, and the number of functional teeth. Aging results in reduced sensory and motor functions, as well as changes in deglutition function. Reduced tongue muscle strength, tooth loss, and reduced intraoral sensation induce issues in the deglutition process, leading to stationary food bolus and reduced number of deglutition.
Furthermore, during the pharyngeal stage of deglutition, the speed of the peristalsis movement slows down. This results in an increased amount of remnant material and prolonged relaxation time of upper esophageal sphincter, leading to apnea symptoms during deglutition and increased risk of food entering trachea. Impairment of deglutition due to reduced tongue muscle strength is the major cause of aspiration pneumonia, which is a life-threatening condition [28-30]. Deglutition process involves a wide range of sensory movements and interactions with nervous system, and the partial loss of muscle and the nervous system can be improved via rehabilitation, although repetitive exercise is needed [31].
Tongue muscle strength exhibited significant positive correlation with lip muscle strength and the number of functional teeth, and lip muscle strength exhibited significant positive correlation with the number of functional teeth. Lip muscles play an important role in preventing food or liquid from leaking outside of the oral cavity while consuming food [32], and reduced lip muscle strength leads to food leakage on the edges and issues with deglutition and pronunciation [33]. Elderly individuals experience difficulties during meals with food spilling out of their mouth, leading to avoidance of social activities involving meals. Overall, reduced lip muscle strength brings a negative impact on their quality of life. It has been suggested that lip muscle strength is associated with gripping force and that reduced lip muscle strength is associated with difficulties in deglutition [34], although future studies are needed for further discussion.
Changes in oral myofunction with aging causes reduced strength of the muscles near the oral cavity including the masticatory muscle that provides masticatory function and the tongue and lip muscles that provide deglutition function. Reduced masticatory function leads to limited types of food consumption, bringing negative effects on physical and mental health due to consequent malnutrition, avoidance of social meals, and stress [35].
Masticatory, tongue, and lip muscles work together to grant masticatory, deglutition, and pronunciation functions of the oral cavity, by providing oral motor movement and ensuring correct position and occlusion of the teeth. Therefore, the importance of oral myofunction for maintenance of appropriate oral function should be highlighted [36]. Specifically, the deglutition impairment in elderly populations is a major cause of reduced oral health-related quality of life. To prevent these issues from arising, systematic processes including exercises to improve oral myofunction should be established. In the field of occupational therapy there are interventions to treat the impairment of deglutition. Since mastication and deglutition are the key functions of the oral cavity, dental hygienists should be trained to address these issues and universities or colleges should provide adequate training for these dental hygienists. Lastly, comprehensive studies to help the elderly population with the recovery of oral function should be more actively performed in the future.
This study has suggested the importance of maintaining oral myofunction for a healthy oral condition in the elderly population as well as the correlations among oral myofunction, oral environment, and cognitive function. Despite these interesting findings, there are limitations to this study. First, since this study was based on a small cohort of elderly subjects from a local community, it is difficult to generalize the outcomes to the entire Korean population. Future studies should be performed on larger cohorts of diverse subjects. Second, since the importance of oral myofunction is not well recognized in Korea, intervention programs and educational sessions to maintain and improve oral myofunction should be established. Future studies should objectively demonstrate the improvement of oral myofunction via these established programs. Nevertheless, this study had a novel approach to understand the correlation between cognitive function and oral myofunction. Additional studies should be performed to increase the awareness of maintaining oral myofunction—which affects mastication, deglutition, and pronunciation—to contribute to the improvement of oral function in the Korean population.
Conclusions
This study assessed correlations among oral myofunction, oral environment, and cognitive function in a cohort of 60 elderly subjects ≥65 years old from a senior nursing home daycare center in the city (N) and a senior center at an apartment in the city (D) between November and December 2018. The following are the conclusions of this study:
1. For oral myofunction according to age, both tongue muscle and lip muscle strengths were greater in the group of <81 year old elderly subjects (38.99±8.51; 10.44±3.50) compared to the group of ≥81 year old elderly subjects (34.85±7.84, p>0.05; 8.50±2.56, p<0.05).
2. For oral myofunction according to the number of functional teeth, both tongue muscle and lip muscle strengths were greater in the group with ≥15 functional teeth (40.91±7.36; 10.54±3.40) compared to the group with <15 functional teeth (32.52±7.14; 8.20±2.41, p<0.05).
3. Both tongue muscle and lip muscle strengths of the subjects with mild cognitive impairment (32.89±7.87 and 8.52±1.39) were weaker compared to the normal elderly subjects (40.80±6.84, p<0.001; 10.28±4.14, p<0.05). In addition, the number of functional teeth was also lower in the subjects with mild cognitive impairment (10.42±9.79) compared to the normal elderly subjects (18.24±9.20, p<0.05).
4. Correlation analyses among oral myofunction, oral environment, and cognitive function have shown significant positive correlations between cognitive function and tongue muscle strength (r=0.478, p<0.001), lip muscle strength (r=0.281, p<0.05), and the number of functional teeth (r=0.386, p<0.001). Tongue muscle strength had significant positive correlations with lip muscle strength (r=0.360, p<0.001) and the number of functional teeth (r=0.633, p<0.001). Lastly, a significant positive correlation was observed between lip muscle strength and the number of functional teeth (r=0.376, p<0.001)
As shown above, the age and the number of functional teeth were found to have effects on oral muscle strength, and elderly individuals with mild cognitive impairment had fewer number of functional teeth and weaker oral muscle strength. These findings imply the need for the development of programs that promote maintenance of oral hygiene and muscle strength from young adulthood to improve oral health-related quality of life in aging societies.