Introduction
Dementia affects brain function; its causes are unclear, and it is not cured. The disease is characterized by loss of various bodily functions, including memory. Because patients with dementia experience difficulties with managing activities of daily living by themselves, they require various medical services and assistance from others [1]. The elderly population in Korea with dementia was estimated to be around 570,000 in 2013, accounting for 9.4% of the total elderly population [2]. The number is expected to increase to 1.01 million by 2024, and as a result, caring for elderly with dementia has emerged as a major health care concern [2]. Dementia is no longer an individual problem, and the Dementia Control Act was legislated by the government in order to reduce individual pain and suffering as well as societal burden [3]. According to the articles 1 and 3 of the Dementia Control Act, national and local governments should actively put in efforts to prevent dementia and provide proper medical service for dementia patients by implementing and supporting dementia management projects, and also offer programs such as dementia research projects, dementia examination projects, and family support projects for dementia patients [4]. Accordingly, the Korean government implemented various national level measures, including the announcement of the “National Responsibility System for Dementia” in 2017, further expansion of the long-term care insurance system for the elderly, and establishment of dementia centers nationwide [5,6].
Among various problems that patients with dementia, many problems are related to oral health. Patients with dementia experience difficulties with oral hygiene care and are vulnerable to various oral diseases, such as dental caries and periodontal diseases, while there are many patients with dementia who suffer because of this [7,8]. However, oral health approach related to dementia till date has not been up to par and despite many existing articles and studies emphasizing the association between dementia and poor oral health [9-12], there is still a lack of interest and countermeasures on this matter. Dental professionals providing oral health care to patients with dementia must understand the characteristics of patients with dementia and have the skill to effectively communicate with the patients, while also needing detailed strategy for coping with behavioral disorders [13]. However, current education on patient care for those with dementia mostly focusses on nursing professionals, while education for dental professionals is still lacking [14]. Despite the fact that dental hygienists can make the biggest contributions to providing professional oral health to patients with dementia [15], they are still unprepared. If dementia-related education is not properly provided in the undergraduate programs, it can lead to lack of appropriate knowledge and will negatively affect elderly with dementia [16]. Therefore, dental hygiene degree programs must provide systematic education that contain proper knowledge and positive attitude towards dementia, which would allow the students to grow into professionals, who can provide oral health intervention to patients with dementia. However, in a study was conducted in 2012 on the standard curriculum for dental hygiene in Korea [17], dementia was not discussed in detail. Currently, although some of the subjects covering geriatric health are offered, dementia-related education is not being offered properly in the dental hygiene degree program in Korea [18,19], and there are no clear legal regulations on related work. Moreover, previous studies reported high educational needs for dementia among professors and students of dental hygiene and dental hygienists [18,19]. The present study aimed to investigate the current state of dementia-related education for dental hygiene degree programs in Korea and dementia-related education for other health care-related majors to derive at the current problems in dementia-related education and to develop a dementia-related curriculum through consultation and assessment by an expert panel.
Methods
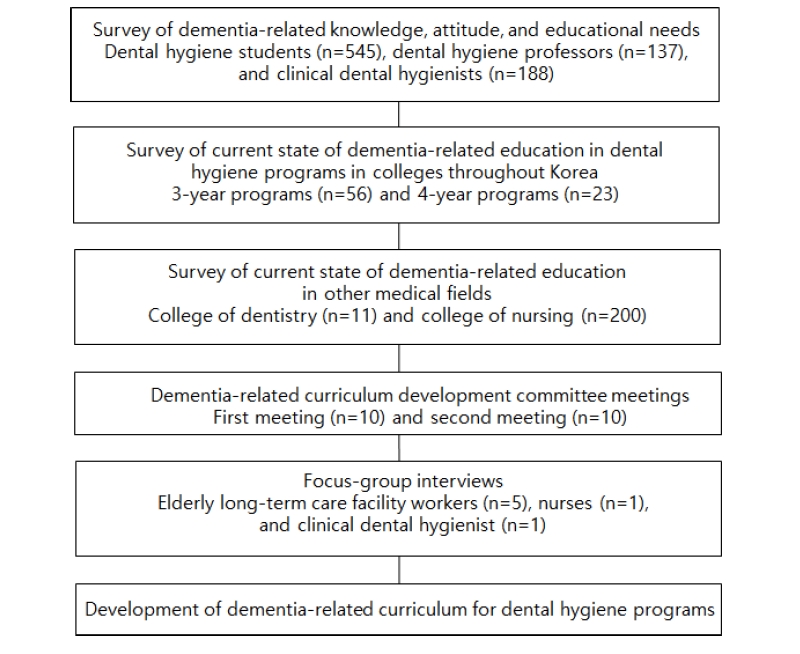
The present study was conducted between April and November of 2018 with the approval of the institutional review board (SHIRB-201804-HR-061-02) of the Shinhan University, and the procedures are as shown below <Fig. 1>.
1. Basic content of preliminary curriculum
First, a preliminary study was conducted to survey dementia-related knowledge, attitude, and educational needs in dental hygiene students (n=545); professors of dental hygiene (n=137); and clinical dental hygienists (n=188) [18,19]. Subsequently, the current state of dementia-related education in dental hygiene colleges throughout Korea and dementia-related education for other health care-related fields were surveyed. Based on the study results, the basic content for the preliminary curriculum was constructed.
2. Formation of a curriculum development committee
A dementia-related curriculum development committee consisting of 10 professors of dental hygiene who are active members of Korean Dental Hygienists Association, Korean Association of Dental Hygiene Professors, and Korean Society of Dental Hygiene was formed. In the present study, the members of the curriculum development committee played a role as decision-makers based on the authority given to make decision on the operation and details of the dementia-related courses. The selection of the details of dementia courses was based on items contained in the 2009 Seoul Metropolitan City Dementia Management Project Educational Resource Book (Citizen’s Dementia Prevention Education) [20], which were decided through content validity assessment conducted by the committee members. The researchers played the role of intervening in the curriculum development committee meetings, logging the details of the meetings, and compiling and organizing the opinions derived. The curriculum development committee meetings were held twice. The contents from the first meeting were reviewed and re-discussed, after which, the operation and details of dementia-related courses were constructed.
3. Expert panel assessment
The operation and details of the developed dementia-related courses were assessed and revised based on focus-group interviews with workers in elderly long-term care facilities, nurses, and clinical dental hygienists. For the staff of nursing homes, directors and care workers taking care of elderly with dementia at nursing homes and home care facilities located in Seoul-si and Gyeonggi-do were selected. A nursing professor currently teaching at a university was selected as a nursing specialist, and a clinical dental hygienist with 25 years of work experience was also selected for the study. The focus group interview was conducted twice, and the objectives, study methods, and recording of interviews were fully explained to the participants before the interview. Each interview took about 2 hours, and the focus group interview was conducted in a lecture room at the researcher’s university. The interviews were recorded after getting consents from the participants. After the 1st interview, there cordings were transcribed and summarized for data analysis, and the contents for the 2nd interview were designed based on this analysis.
4. Development of dementia-related curriculum
Opinions derived from the curriculum development committee and expert panel assessment results were used to develop the dementia-related curriculum for dental hygiene.
Results
1. Current state of dementia-related education in dental hygiene degree programs
A review of the current state of dementia-related education in dental hygiene degree programs found that out of 56 3-year and 23 4-year dental hygiene degree programs, not a single school offered a major course with the term “dementia” in the course description. One school had a general education course with the term “dementia,” which was “elderly health and dementia.”
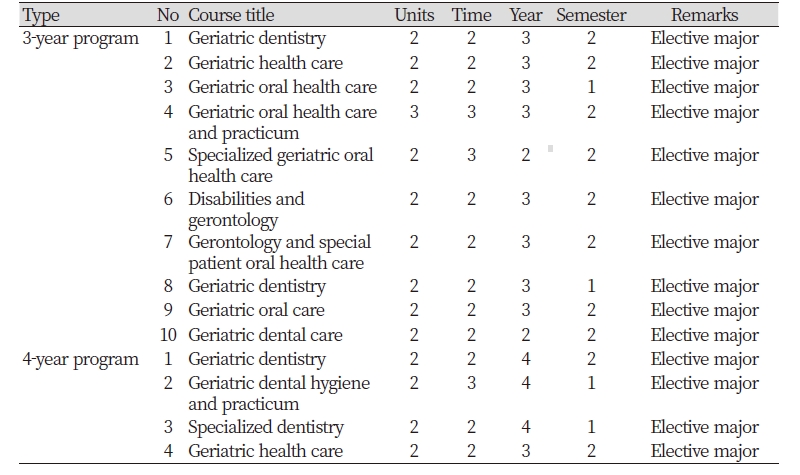
The number of schools with courses that included content on geriatric and systemic diseases and special patient care, which have a relatively high association with dementia was 10 3-year (17.9%) and 4 4-year (17.4%) schools <Table 1>. The course names appeared as geriatric dentistry, geriatric health care, and geriatric oral health care, while only 1 3-year and 1 4-year schools included practical lessons. The number of units and instructional hours of related courses were mostly 2 units and 2 hours, respectively, and the courses were being offered mostly during the third year in vocational colleges (3-year program) and fourth year in regular colleges (4-year program).
Table 1. Current state of dementia-related courses offered in oral hygiene programs throughout Korea
|
2. Current state of dementia-related education in other fields
1) College of dentistry
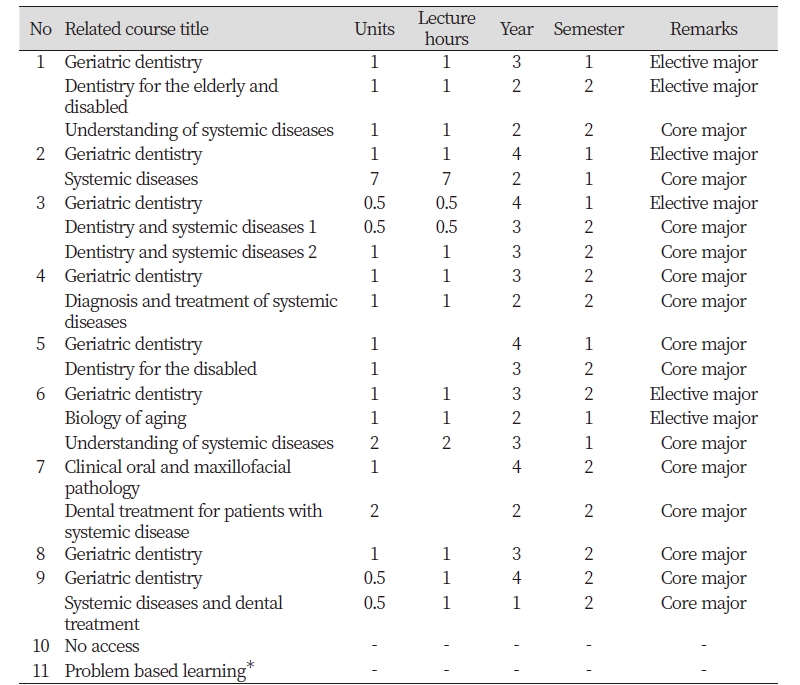
A review of the current state of dementia-related education in colleges of dentistry found that among 11 colleges of dentistry throughout Korea, 10 colleges allowed access to their curriculum. Among these 10 colleges, there were no schools that offered any major, elective, or general education courses that contained the term “dementia.” Moreover, dementia-related courses being offered were as shown below <Table 2>.
Table 2. Current state of dementia-related courses offered in college of dentistry throughout Korea
|
|
|
* Because the course is operated by combining various courses, a separate course title is not given |
|
Related course names appeared mostly as geriatric dentistry and understanding of systemic diseases. Most of the courses were 1-unit courses, which were often classified as core major courses. The courses were being offered at various stages of the program, from the first semester of first year to second semester of fourth year.
2) College of nursing
A review of the current state of dementia-related education in colleges of nursing found that among 200 or more colleges of nursing currently in Korea, there was no school that offered any major or elective courses that contained the term “dementia.” Furthermore, while there were differences between colleges on related courses offered, education on dementia or Alzheimer’s disease was being offered, 1 session each, in adult nursing or psychiatric nursing (core major courses) or geriatric dentistry (elective major course). Moreover, colleges that were designated as leading colleges for overcoming dementia were offering such courses as 1-unit required general education courses.
3. Dementia-related curriculum development committee
1) Educational content
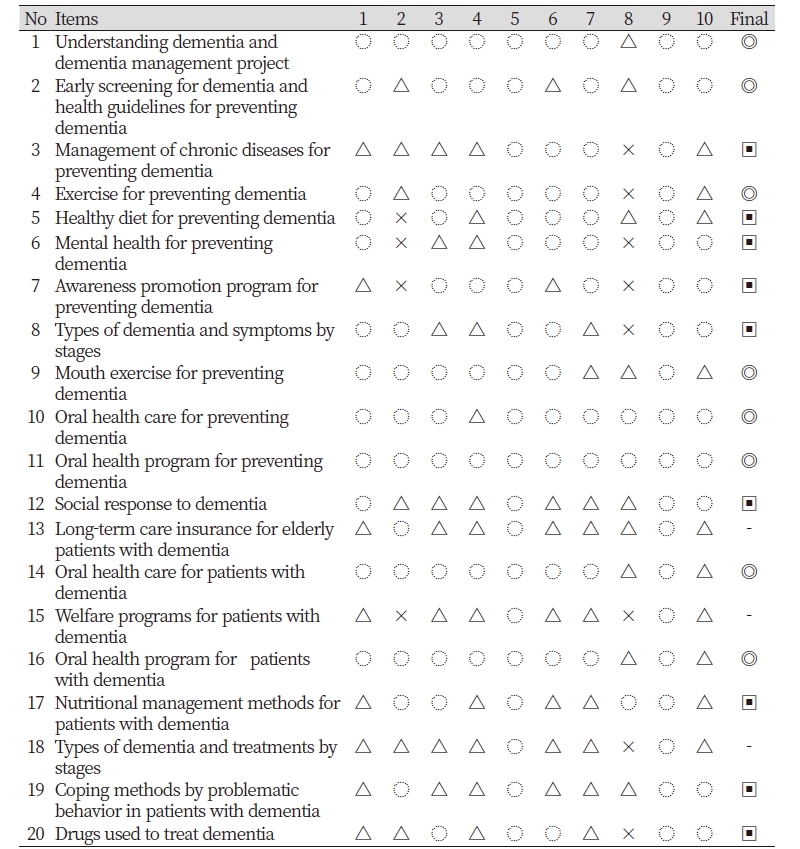
The educational content derived by the curriculum development committee was as shown in <Table 3>.
First, the committee was asked to express their opinions on mandatory, elective, and unnecessary items based on an assessment of curriculum, consisting of 20 items. Based on the derived results, items for which 7 or more members responding it was required were classified as “required education content,” while items with 4-6 members responding it was required were classified “elective educational content” and if 3 or fewer members responding it was required , they were classified as “unnecessary educational content.” Subsequently, the items selected as “required educational content” included a total of 8 items: “understanding of dementia and dementia management project,” “early screening for dementia and health guidelines for prevention of dementia,” “exercise for prevention of dementia,” “mouth exercise for prevention of dementia,” “oral health care for prevention of dementia,” “oral health programs for prevention of dementia,” “oral health care for patients with dementia,” and “oral health programs for patients with dementia.” In addition, 9 “elective educational content” items and 3 “unnecessary educational content” items were selected.
2) Operational types of dementia-related curriculum
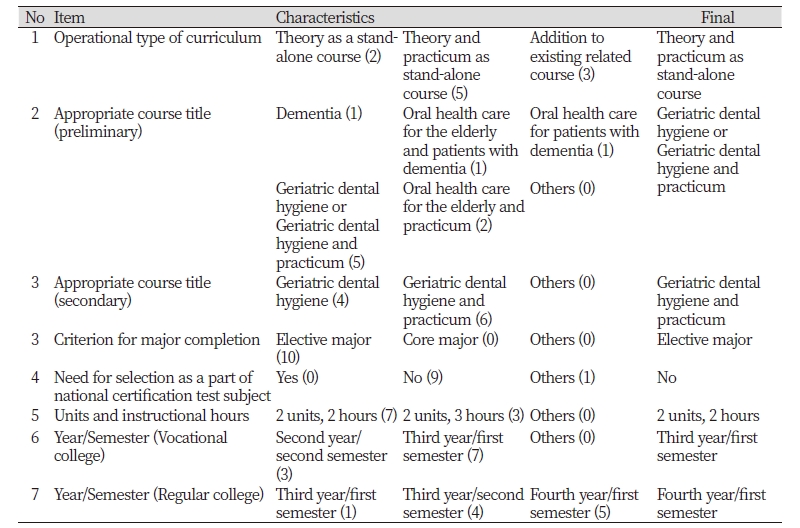
The dementia-related curriculum development committee decided to operate the curriculum as a stand-alone course with theoretical and practical lessons. The name of the curriculum was determined to be “geriatric dental hygiene or geriatric dental hygiene and practicum” based on the preliminary meeting, where 5 members voted on the name. In the second meeting, the name was ultimately decided to be “geriatric dental hygiene and practicum.” The goal of this course was to learn the method of managing and understanding the characteristics of the elderly and consensus was reached to operate some theoretical and practical lessons on dementia-related content. The criterion for completion of major was selected as “elective major” and most members voted “no” on whether it should be selected as part of the national certification test subject. The units and instructional hours for the course were set as 2 units and 2 hours, respectively. It was decided that the course would be offered during the first semester of third year for vocational colleges (3-year program) and first semester of fourth year for regular colleges (4-year program) <Table 4>.
4. Expert panel assessment
When the operation and details of the dementia-related curriculum derived from the curriculum development committee were assessed through focus-group interviews, there were no disagreements about the operation of the curriculum. However, based on the assessment, it was determined that “managing dysphagia for patients with dementia” and “coping methods for problematic behavior of patients with dementia,” which were classified as “elective educational content” should be classified as “required educational content.” Moreover, some opined that in addition to theoretical lessons in lecture rooms, it would be important to gain practical experience through talent donation activities and field experience targeting community-dwelling elderly.
5. Development of dementia-related curriculum for dental hygiene degree programs
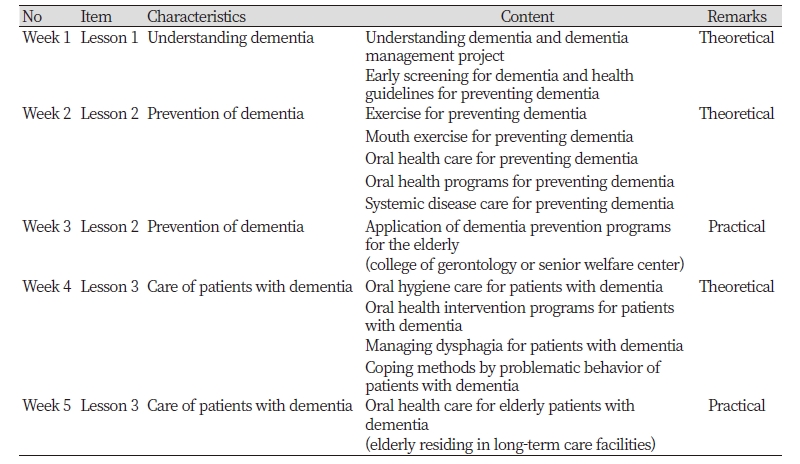
The dementia-related curriculum developed for dental hygiene degree programs was as shown in <Table 5>.
The operation of the dementia-related curriculum remained exactly as determined by the curriculum development committee, without any revisions. However, by accepting the assessment results of the expert panel, “managing dysphagia for patients with dementia” and “coping methods for problematic behavior of patients with dementia” were classified as “required education content” to bring the number of “required educational content” items to a total of 10.
The dementia-related education comprised a total of 3 instructional sessions of “required educational content” with 3 weeks of theoretical lessons and 2 weeks of practical lessons (1 session at college of gerontology or senior welfare center and 1 session at elderly long-term care facility). In addition, “elective educational content” or dementia-related talent donation activities were set to be taught according to the actual situation of each college.
Discussion
The number of patients with dementia among the elderly population is rapidly growing worldwide, and as a result, the percentage of elderly with dementia in long-term care facilities is expected to increase [21]. Accordingly, dental hygienists will face more opportunities to encounter elderly patients with dementia who have different combination of various symptoms, including cognitive and/or behavioral impairment in dental clinical practice or the community [22,23]. However, despite the fact Korea is on the cusp of becoming an aged society, establishing oral health policies and activities in patients with dementia are still lacking. Even dental clinics are not equipped with programs that can prevent dementia in the elderly or provide professional intervention for patients with dementia [24].
An examination of the current state of dementia-related education in dental hygiene degree programs in Korea revealed that there were no colleges that offer any major course that contained the term “dementia.” Moreover, colleges that offered dementia-related courses accounted for only 17.9% of all 3-year colleges and 17.4% of 4-year colleges, which was in contrast to colleges of dentistry offering dementia-related courses as core major courses. This was also in contrast to colleges of nursing providing standardized education on dementia or Alzheimer’s disease to their students.
Application of dementia education program, practical lessons on geriatric nursing, and nursing experience has an effect on improving the knowledge of and attitude towards elderly patients with dementia among nursing students [25,26]. A high rate of burnout among nurses who care for the elderly is associated with having a negative attitude towards elderly patients with dementia and problems sometimes arise due to misunderstanding about dementia-related behavioral impairment faced while caring for patients with dementia [27]. Therefore, dental hygiene education must include proper knowledge of and positive attitude towards elderly patients with dementia. In addition, it is also necessary to learn oral health intervention for patients with dementia, but also the methods for understanding and coping with problematic behavior of patients with dementia.
The duties of dental hygienists vary slightly from country to country, but to at least acquire professionalism in oral health intervention in an aging society, education on the subject matter is necessary. However, there have very few studies on dementia-related education for dental hygienists and oral health intervention for patients with dementia to date, with most of the studies focusing on intervention for nurses and caregivers [9,28,29]. Furthermore, according to a 2005 survey of dentists [30], most dentists responded that education on special care patients was not conducted properly in their undergraduate dentistry program. Therefore, it was determined that education for patients with dementia among dental professionals is inadequate.
Hopcraft et al. [31] claimed that dental hygienists can establish proper dental hygiene care plans for elderly patients in long-term care facilities and that it would be beneficial to increase the utilization of dental hygienists in increasing the safety and efficiency of providing dental care services to elderly patients in long-term care facilities. Currently in Korea, article 2 of the Medical Technician Jurisprudence stipulates that the duties of dental hygienists shall be defined as scaling, fluoride application for dental caries, prevention of dental and oral diseases, and hygiene-related work under the direction of a dentist [32]. Therefore, it is believed that oral health intervention for patients with dementia also falls within the work scope of dental hygienists. In the present study, a consensus was reached to operate theoretical and practical lessons for the course titled “geriatric dental hygiene and practicum” as a part of the dementia-related curriculum (proposed). Currently, a course on “community oral health and practicum” is offered as a part of dental hygiene curriculum, but education about the elderly in this course is extremely limited to some theoretical and practical lessons, and thus, establishment of separate courses is deemed necessary. Required educational content consisted mostly of understanding and prevention of dementia and oral health care of patients with dementia, and based on the expert panel assessment, “managing dysphagia for patients with dementia” was also added. In this regard, in Japan, where patients with dementia are relatively well-managed due to being the fastest country to have an aging society, dental hygienists gain theoretical knowledge about the characteristics of the elderly, but they also personally learn methods and techniques for providing care to the elderly [33]. Therefore, the curriculum developed in the present study was constructed with consideration for oral health care of patients with dementia, along with their systemic characteristics.
For geriatric patients with dementia, elderly long-term care facilities in Japan focus on managing dysphagia, and in such case, a “team approach” involving dentists, dental hygienists, physicians, speech therapists, and occupational therapists is taken [33]. However, elderly long-term care facilities in Korea are more concerned about simply increasing the number of patients being serviced and facility infrastructure, while facing problems with lack of human resources for providing the necessary services, frequent turnover, and overlapping services between different entities [34]. Moreover, despite the fact that Korea now has over 70,000 dental hygienists, they are not allocated to elderly long-term care facilities or welfare centers [35], and even dental hygienists stationed in community clinics or health sub-centers lack professional education, which is expected to show significant differences among individuals on the ability to provide oral health intervention for patients with dementia. Therefore, the most important aspect of operating the curriculum developed in the present study is to implement a unified and standardized education for all dental hygiene programs throughout Korea. For this, continued information sharing and discussions with relevant organization, such as Korean Dental Hygienists Association and Korean Association of Dental Hygiene Professors, are needed, while improved awareness among professors of dental hygiene who are in the frontline of such education is also needed. Moreover, institutional support through discussions with relevant agencies, such as the Ministry of Health and Welfare and Ministry of Education, to allow dental hygienists to provide professional oral health intervention to patients with dementia.
Although additional studies may be needed to confirm and decide on the curriculum developed in the present study, but the present study was significant in that it developed a curriculum with consideration for the social characteristics of Korea and the actual duties of dental hygienists. However, the present study had the limitation of not actually applying the developed curriculum. Moreover, because of a lack of studies on the current state of dementia-related education for dental hygienists, comparative analysis against other study results was inadequate. Therefore, it is necessary to conduct future studies, in which the develop curriculum is actually applied and problems and improvement measures are identified. In the follow-up studies, curriculums that can be effectively applied in the dental hygiene programs need to be developed through the evaluation and in-depth discussion of our study results by education specialists. It is expected that future studies based on the findings in the present study will be actively pursued.
Conclusions
The objective of this study was to examine the current state of dementia-related education for dental hygiene degree programs in Korea as well as to develop a dementia-related curriculum for dental hygiene programs that is suitable for the social characteristics of Korea. The study was conducted between April and November 2018. First, the current state of dementia-related education for dental hygiene programs in colleges throughout Korea and dementia-related education for other health care-related fields were investigated. Based on the initial findings, the basic content of the preliminary curriculum was constructed. Second, based on the opinion of the dementia-related curriculum development committee comprising 10 professors of dental hygiene, the operations of dementia-related courses and relevant details were constructed. Third, these operations and relevant details were assessed and revised based on focus-group interviews. Fourth, the dementia-related curriculum was developed based on the study findings and literature review.
1. The name of the course in the developed curriculum was set as “Elderly Dental Hygiene and Practicum.” The course was established as a “major elective,” and was offered as two units with two instructional sessions of two hours each.
2. The learning goal for this course was acquiring the methods for understanding and managing the characteristics of the elderly. A consensus was reached regarding conducting the theoretical and practical lessons on some of the dementia-related content.
3. The dementia-related curriculum comprised 10 “required contents” which is to be conducted over three weeks of theoretical lessons and two weeks of practical lessons.
With the growing elderly population, the development and operation of the curriculum for geriatric oral health interventions are warranted in dental hygiene education. However, continued discussions and improvements are needed on the extent of educational content, considering various dementia-related symptoms and general geriatric systemic diseases.