Introduction
Periodontal disease and dental caries were the 5th most expensive medical expenses in the first half of 2021 in Korea. Since the statistical cost index includes systemic diseases, this ranking is quite high[1]. This means that treatment-oriented dental services are being prioritized over preventive care. In addition, the cost of dental treatment is increasing due to this.
According to the 2018 Korean National Children’s Oral Health Survey, More than half of 12-year-olds have experienced dental caries, and the average number of decayed tooth by 12-year-olds was 1.84, higher than the average of 1.2 in OECD member countries. These statistical results suggest that more than half of school-age children suffer from dental diseases, such as dental caries; thus, awareness of oral health requires improvement [2].
Dental plaque can lead to serious oral disease [3-6]; to prevent disease, various oral care tools are used to manage these dental plaques, but it is difficult to manage them completely [7,8]. In addition, although knowledge about health can be improved using existing health education methods [9,10], knowledge alone does not change oral health behaviors [11]. Augmented reality is being used in various fields such as education and medicine that require behavioral change, and its effectiveness is gradually increasing [12,13].
Brushing not only improves aesthetics by cleaning food residues left behind during eating and drinking, it refreshes the oral cavity and prevents dental plaque formation and acid production [14]. Its mechanical action removes already formed and attached dental plaque, and it is the most commonly used oral health care behavior in daily life [15]. Therefore, it is very important to develop correct behavioral habits to encourage lifelong oral health management, ideally from childhood [16,17]. In addition, children should form good habits before their permanent teeth erupt so that they can maintain a healthy oral condition for the rest of their lives [18,19].
AR-based education provides a rich learning environment [20] because it includes additional virtual learning information and enables self-directed experiential learning by allowing direct manipulation using the learner’s various senses [21-23]. Tooth brushing education requires instruction on the area to be brushed accurately and education on how to brush, and education through video or real objects is effective. Toothbrushing instruction requires on tooth area to be brushed accurately and education on how to brush [24], and in non-face-to-face education, tootbrushing education is conducted through video media, or in face-to-face education, education is conducted through real objects such as tooth models and toothbrush [25,26].
Since AR encourages induces users to act naturally and actively interact with virtual images, in this case in a brushing habit-forming application, users can continuously and voluntarily develop appropriate toothbrushing and oral health care behaviors.
The purpose of this study was to evaluate whether plaque removal efficiency could be improved through toothbrushing using an AR guide program designed to help learning to brush teeth properly by utilizing the advantages of AR.
Methods
1. Study subjects
The feasibility study was designed using two period cross-over design. This study included 20 subjects residing in C city for people aged by 5-12, who agreed them and their parents to participate after understanding the purpose and contents of this study. This study was approved by the Institutional Review Board (IRB approval No.: S-D20220008) and was conducted in accordance with the ethical standards of the Declaration of Helsinki. The number of samples was calculated using the standard deviation of previous studies, and the total number of samples was calculated as 20 considering the reliability of 90% and dropout rate of less than 10% [14].
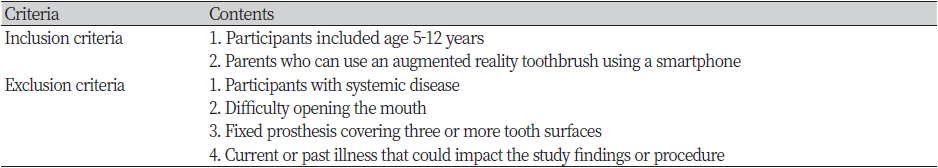
2. Subject inclusion and exclusion criteria
1) Inclusion & exclusioncriteria
2) Criteria for subject discontinuation and withdrawal
The present study could be discontinued or subjects could withdraw if they did not comply with or violated items stated in the written informed consent form, if unpredicted severe complications occurred, or if a researcher or the principal investigator deemed a subject inappropriate for continued study participation.
3) Subject identification
Subjects who met the inclusion and exclusion criteria specified in the study protocol and whose parents provided written informed consent were assigned a unique identifier, formatted as YDF-18##, that was recorded on the corresponding case report form.
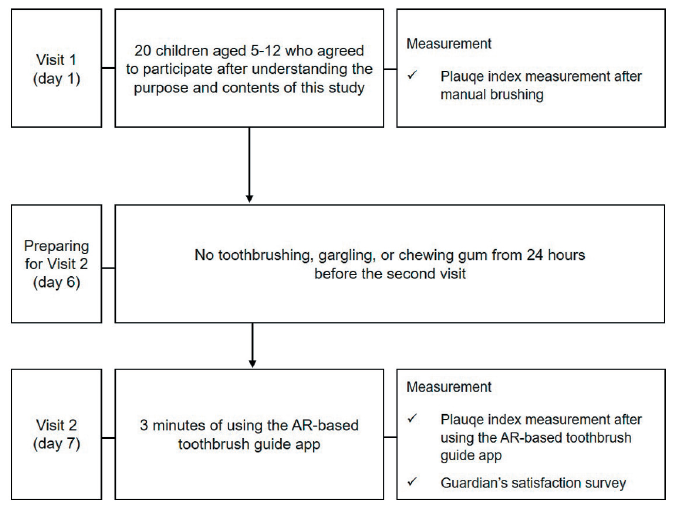
4) Overview of study procedures
The present clinical evaluation used a crossover design as described below.
5) The clinical study procedure
(1) Preparations
This randomized doubleblind clinical study was designed to evaluate for smart brush. During the screening process, the subject’s appropriate oral health condition and written consent were obtained, and evaluation was performed using a manual toothbrush, and brushing was standardized by the Fone’s method. After that, at the second visit, dental plaque removal effect after using the smart toothbrush was evaluated, and compared with that of first visit.
6) Observation items and clinical exams
(1) Plaque index test
A disclosing solution (Trace, Disclosing Solution; Young Dental, Earth City, MO, US) was applied to all erupted teeth, and plaque deposit intensi-ties and locations were observed.
After cleaning of all tooth surfaces dried using air syringe, the disclosing solution was applied using cotton pellets moistened with the solution. Once the surfaces of the teeth had been dried, they were evaluated using the Patient Hygiene Performance (PHP) index. The following tooth surfaces were evaluated: buccal surface of the maxillary right first molar, labial surface of the maxillary right central incisor, buccal surface of the max-illary left first molar, lingual surface of the mandibular right first molar, labial surface of the mandibular left central incisor, and lingual surface of the mandibular left first molar.
(2) Use of a smart toothbrush
Brush Monster Toothbrush <Fig. 2>, an augmented reality, recognizes the location of the toothbrush through a smart device, and based on this, a guide for the user’s brushing area is followed on the smartphone. Through game-based content, it guides you in getting rid of germs in your mouth so that you can brush your teeth without missing parts.
Tailored education was provided using a smart toothbrush. Each child used their dominant hand regardless of side and had the option of choosing a toothbrushing technique (scrub, Fones, or Bass). Based on the tailored education, the children could not only develop an effective toothbrushing technique, using a total of 16 steps, from brushing the teeth in the order of occlusal, buccal, and lingual surfaces (starting from the occlusal sur-face in the mandibular left and ending at the lingual surface in the maxillary right), but they were empowered to do everything on their own from the beginning to the end of the toothbrushing process (from squeezing toothpaste on the toothbrush to washing the cup). Each subject was provided a Brush Monster, and after they completed the training.
The AR-based smart toothbrush used in the present study was intended to instruct the children how to correctly brush step by step.
3. Statistical Analysis
The study used two period cross-over design. This study measured tooth-brushing performance and time and oral hygiene using manual toothbrush and after using smart toothbrush. The paired t-test and two groups t-test was used to determine the significant difference in tooth-brushing performance and each test-outcome variable within a group. Statistical significance was set at p<0.05. All statistical analyses were conducted using the IBM SPSS program (ver 26.0; IBM Corp., Armonk, NY, USA).
Results
1. Outcome assessment
1) Study subjects
A total of 20 children without any prior toothbrushing education participated in the present study. Of them, 12 were boys and 8 were girls; 9 were 5 years old; 2 each were 7, 8, and 9 years old; and 1 was 10 years old. The mean participant age was 6.35 years.
2) Assessment of changes in dental plaque
(1) Overall assessment
The visit 1 assessment of the effects of manual toothbrushing in the 20 subjects showed that the mean PHP index score decreased from 20.30 points (±3.73) before toothbrushing to 13.35 (±5.08) after. After a 6-day washout period, the effects of the AR-based vibrating toothbrush used in conjunction with the associated educational pro-gram were assessed during visit 2. The mean PHP index score decreased from 22.00 (±3.63) before toothbrushing to 6.35 (±6.19) after toothbrushing <Table 2>.
|
Table 2. Comparison of changes in dental plaque index between manual toothbrush and AR guided toothbrush 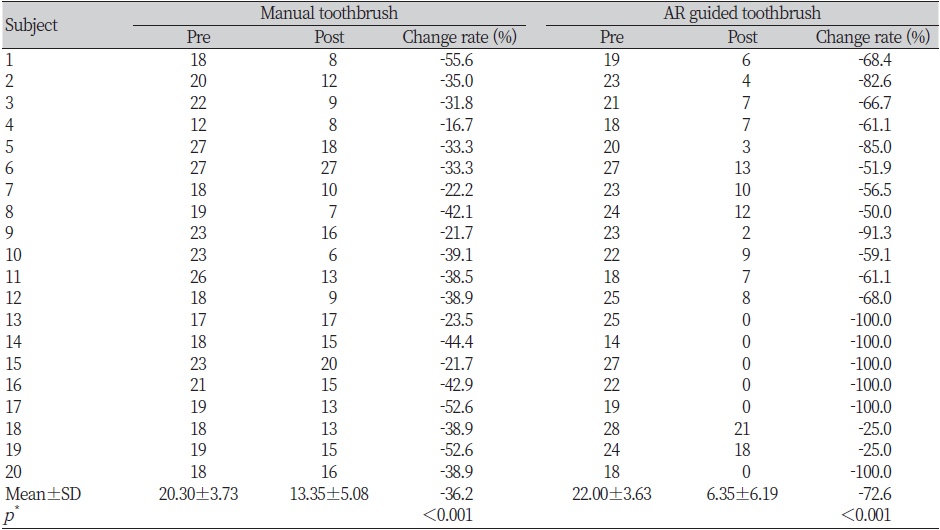
|
|
*by paired t-test, AR: augmented reality |
Comparison of plaque removal efficiency between the Brush Monster and the manual toothbrush showed that the PHP index score decreased by an average of 15.65 and 6.95 points, respectively. The mean plaque removal rate with the Brush Monster was 72.6%, approximately twice as high as that for the manual toothbrush (36.2%, p<0.05).
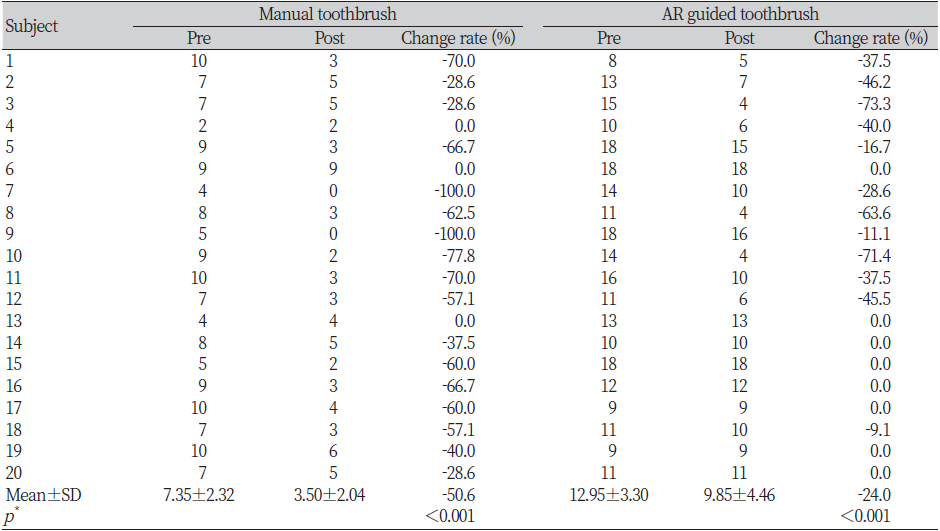
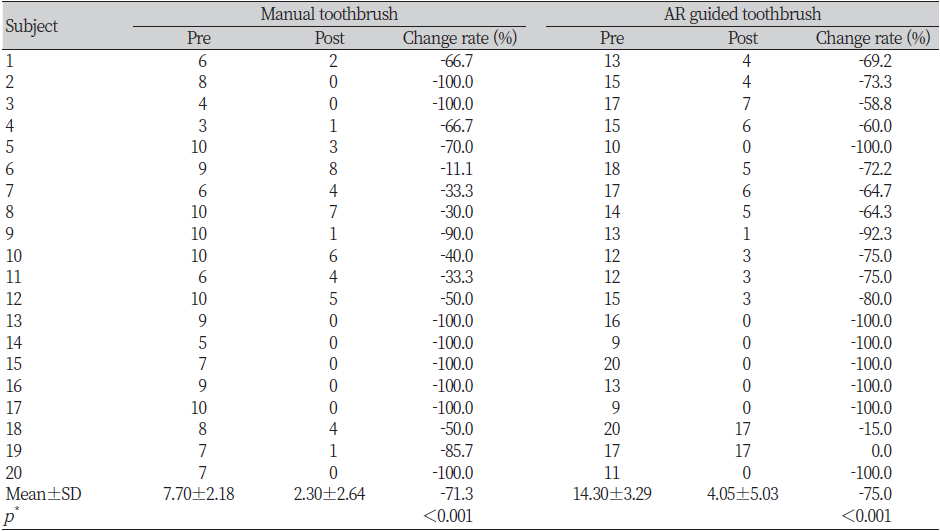
(2) Assessment of anterior and posterior teeth
The plaque removal effects of the Brush Monster versus manual brushing were as-sessed separately for the anterior and posterior teeth. In the anterior teeth, the mean PHP index score was 7.35 points (±2.32) before and 3.50 (±2.04) after manual brushing, show-ing a decrease of 3.85 points. In the posterior teeth, the mean was 12.95 (±3.30) before and 9.85 (±4.46) after manual brushing, showing a decrease of 3.10 points <Table 3>. The plaque removal effects of the AR-based vibrating toothbrush, however, were as follows: In the anterior teeth, the mean PHP index score was 7.70 (±2.18) before and 2.30 (±2.64) after using the AR-based toothbrush, showing a decrease of 5.40. In the posterior teeth, the mean PHP index score was 14.30 (±3.29) before and 4.05 (±5.03) after using the AR-based toothbrush, showing a decrease of 10.25 <Table 4>. Thus, the difference in the plaque removal effects in the anterior teeth between the manual and AR-based smart vibrating toothbrushes was 1.55 points (±3.41), with the effect being greater for the AR-based tooth-brush, although the difference was not statistically significant (p=0.056). In the posterior teeth, the difference was 7.15 points (±5.65), with the plaque removal effects being greater in the AR-based smart vibrating toothbrush as well, although this difference was statistically significant (p<0.05).
Discussion
Oral health behavior develops in early childhood; accordingly, lifelong oral health habits are influenced, and appropriate education at the relevant time is important [27]. Toothbrushes are also closely associated with tooth loss, periodontal disease, and gum eclipse. These conditions are closely associated with systemic diseases in adulthood, difficulty forming positive oral health management behaviors, and limited ability to perform complicated oral health management processes [28,29].
With the advanced development of extended reality such as augmented reality and virtual reality, the application of ICT technology to health maintenance programs is increasing. ICT technology can be used for tasks such as identifying and tracking oral health problems, helping with diagnoses and treatment planning, assisting with surgical procedures, and predicting patient outcomes. AR-based devices and software are also evolving to help track and analyze oral hygiene habits and provide personalized oral health recommendations. However, the use of AR in oral health is still in its early stages and further research is needed to fully understand its potential and limitations. Therefore, we conducted this study to evaluate the plaque removal effect using apps currently available in the market and to review the applicability.
Until now, AR technology has been mainly applied to the field of oral surgery, but it is gradually expanding to the field of education. Amantini et al [30] conducted a study to train children between the ages of 6 and 10 on how to brush their teeth using AR technology. And it was announced that digital tools using AR have potential effects to motivate oral hygiene practice and improve children’s health awareness. In addition, in the study of a control experiment targeting people with intellectual disabilities, oral hygiene improved significantly in both the AR-based group and the visual data-based education, but the AR-based tooth brushing education was found to be more effective [31].
A comparison of the removal efficiency of the tooth surface dental plaque using the manual toothbrush and the smart toothbrush with the enhanced reality guide showed that the overall tooth surface dental plaque index was significantly reduced. This led to significant results given the fact that guide-based brushing for persons with disabilities with previous behavioral restrictions can better remove dental plaque on the tooth surface and reduce the gingival index [32]. Moreover, it has significance since electric oral management products such as electric toothbrushes and water flossers are useful supplementary oral management tools [33-35]. Regarding changes in child behavior, these AR techniques can be combined with gaming techniques to arouse children’s interest, and these repetitive behaviors and education aid in the establishment of correct health habits [36].
The use of an AR-based smart toothbrush in conjunction with an educational program significantly reduced PHP index scores versus the manual toothbrush in the subjects evaluated in the present study. However, the effects of using the AR-based toothbrush on plaque removal in the anterior teeth were not significant compared to those of manual brushing, while the difference was statistically significant in the posterior teeth. Using the application to watch the person on the screen of the mobile phone, the efficiency of removing dental plaque from the tooth surfaces that are difficult to see with the same plane mirror as the oral cavity is lower than that of the anterior teeth. It is important to brush the teeth without falling into the oral cavity to remove dental plaque, and it is very important to manage the gingival margin or brush the teeth in the lingual direction to prevent oral diseases [37]. Therefore, it is necessary to reinforce special care for parts of the mouth where brushing is ineffective by increasing the time allocated to that area in the brushing guide in the future.
This study could consider the augmented reality-based dental plaque removal effect and usability, but there are some factor in interpreting it. First, the AR app guided brushing methods other than the Fones method, and other brushing methods may have affected the removal of dental plaque. Second, in children who normally brush their teeth for less than 3 minutes, the effect of removing dental plaque may be more evident due to the increased brushing time. Finally, it is difficult to generalize to a small sample. Nevertheless, it is meaningful as there are currently few studies that have confirmed oral health indicators using AR-based apps.
This study secured an appropriate number of research participants based on existing clinical studies, but to generalize our findings, reinforcement is needed further clinical studies are required.
Conclusions
A clinical trial was conducted to investigate the removal efficiency of dental plaque on the tooth surface of an augmented reality-based smart toothbrush.
1. The reduction effect of the overall plaque index seemed to decrease more than when using the augmented reality toothbrush.
2. When the parts devided, there was no significant difference when brushing the anterior part, but there was a significant difference in the removal of dental plaque through brushing in the posterior part.
Through the results of this study, it was possible to confirm the possibility of using augmented reality as a media for toothbrushing education, and it is expected that it can be used as a tool for oral health education as a tool for motivation.