Introduction
According to the “Older Adults Statistics” published by Statistics Korea, 17.5% of the total population of the Republic of Korea is aged 65 years and over as of 2022 [1]. The proportion of older adults doubled from that in 2005, highlighting the country’s rapid aging toward a super-aged society.
Among the measures developed to prepare for this transition, the Korean government launched a pilot program called community care in June 2019, which aims to integrate and provide care, housing, healthcare, long-term care, and independent living support for older adults to promote their healthy living as members of their local communities, as opposed to in hospitals or long-term care facilities [2,3]. The Ministry of Health and Welfare (MOHW) selected eight local governments in 2019 for three different projects (older adults, individuals with disabilities, individuals with mental disorders), with Seo-gu of Gwangju, Bucheon-si of Gyeonggi, Cheonan-si of Chungnam, Jeonju-si of Jeonbuk, and Gimhae-si of Gyeongnam selected for the project for older adults [3]. The home oral care program for older adults, one of the programs offered through the project, was implemented in September 2019 and is still offered in Cheonan-si. The community care project was additionally launched in eight more regions in 2020, totaling 16 regions nationwide [3]. Phase 1 of the project was concluded in December 2022. Phase 2 of the project will be implemented by 12 newly selected local governments from July 2023 to 2025. In response to the results of the National Survey on Older Koreans that “home care” is the most needed survey among older adults, the MOHW expanded a specialized health care program for older adults in 2022 [4] and plans to implement community care nationwide before the country becomes a super-aged society [5]. Thus, the government is paying increasing attention to health problems among older adults, and community caregiving organizations have a growing interest in oral health problems in older adults [6].
Approximately 80% of the older adult population suffers from chronic degenerative diseases and, as their oral health also deteriorates, halitosis is the most common oral symptom observed among older adults [7]. Most cases of halitosis are caused by factors such as poor oral hygiene, poor prosthetic placement, periodontal disease, and xerostomia [8]. Although a coated tongue is the most common cause of halitosis in young adults, periodontal disease is a common cause of halitosis among older adults [9]. Halitosis is a social disorder that can cause discomfort to others and diminishes confidence in individuals with halitosis, adversely impacting their interpersonal relationships and social life [6,7]. Furthermore, halitosis has been associated with mental health concerns such as social exclusion and isolation [10]. Therefore, halitosis is closely linked to the quality of life of older adults, and continuous oral hygiene management by professionals is essential to maintain and improve older adults’ oral health and ultimately enhance their quality of life [11]. Moreover, in addition to professional oral hygiene care and analyzing changes in halitosis using halitosis meters, repeated and continuous oral hygiene education programs must be administered to facilitate rigorous compliance with oral hygiene practices among older adults to improve their oral health. To this end, continuous and integrated management systems tailored to the population structure and regional features must be established to ensure the systematic implementation of community care policies in local communities in Korea, as opposed to professionally managed institutions. [5,12,13].
In this context, this study describes several cases in which home oral care interventions as part of the community care project in Cheonan-si led to reduced halitosis and improved oral health among older adults. The findings will be useful as foundational data for developing tailored home oral care programs.
Cases
1. Study participants
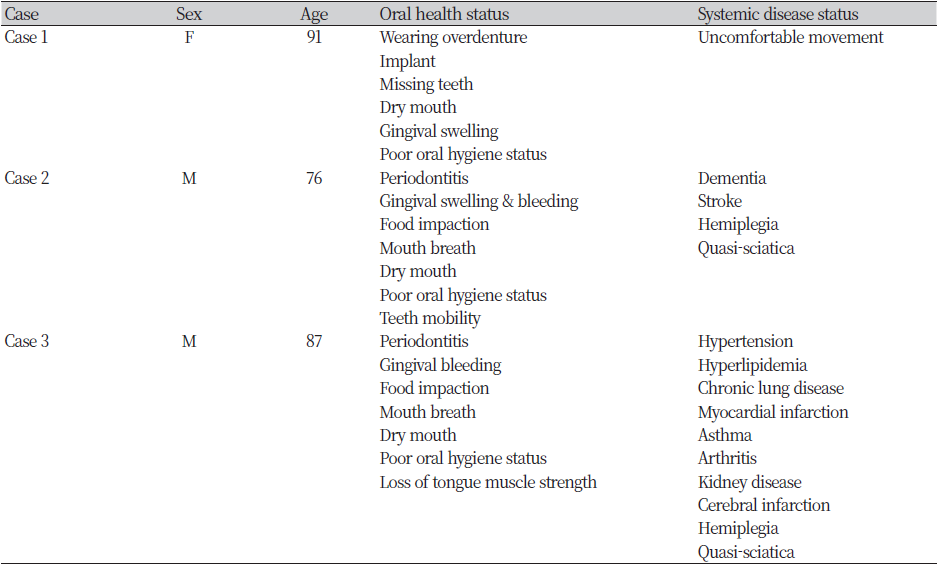
This study assessed the changes in the oral health of older adults with halitosis after home oral care intervention programs administered as a part of the community care project in Cheonan-si, South Chungcheong Province. Of 73 older adults (excluding 25 participants who did not begin or complete the intervention activity for reasons such as being lost to follow-up and withdrawal of enrollment), three individuals with changes in concentration of volatile sulfur compounds (VSCs) after oral hygiene intervention activities were selected to observe the changes in their oral health and measure their concentration of VSCs between March 1, 2022, and January 31, 2023. <Table 1> shows the sociodemographic information of the participants. The study was reviewed by the Institutional Review Board of Dankook University (IRB: DKU 2021-10-010-001).
2. Community care oral health care intervention program
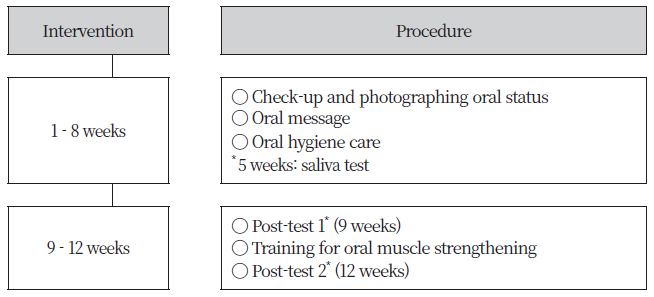
The oral health intervention program is provided by a team of one dentist and 11 dental hygienists divided into two-member home oral health care teams in Cheonan-si. An oral health examination and baseline survey were first conducted, and a 12-week individualized home oral health care intervention program was administered, with one session per week. The oral examination included determining the number of existing teeth, use of dentures, the decayed, missing, filled teeth index (DMFT index), community periodontal index (CPI), plaque index (PI), tongue coating index, and oral status. The baseline survey included halitosis measurement, saliva testing, and questionnaire interview. Halitosis meter measurement and questionnaire survey were conducted on week 9 and week 12 respectively to monitor changes in oral health and concentration of VSCs. <Fig. 1> illustrates the process of the home oral care intervention program.
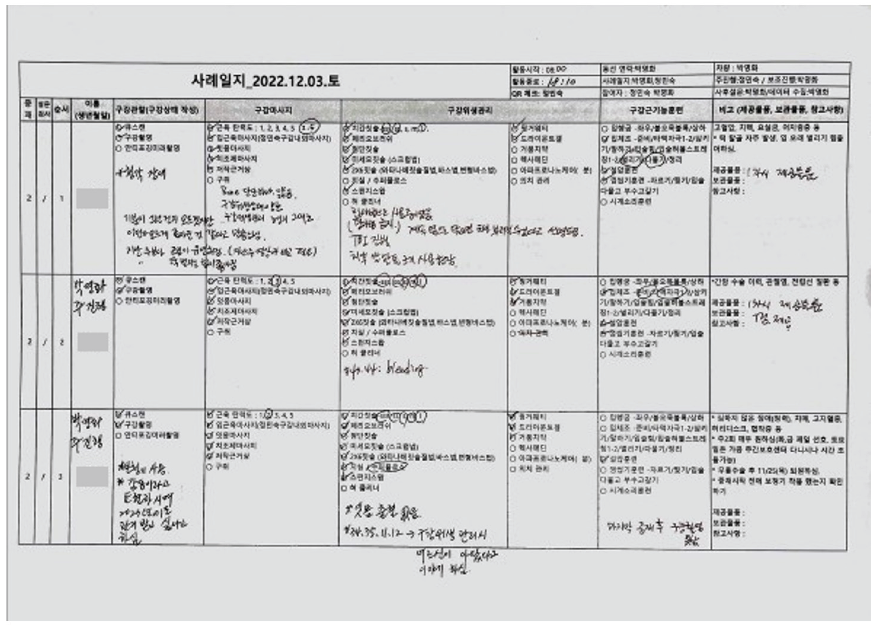
The home oral care team documented patients’ oral health status and their intervention activities every week on their field case notes to monitor changes in oral health throughout the oral hygiene intervention program <Fig. 2>.
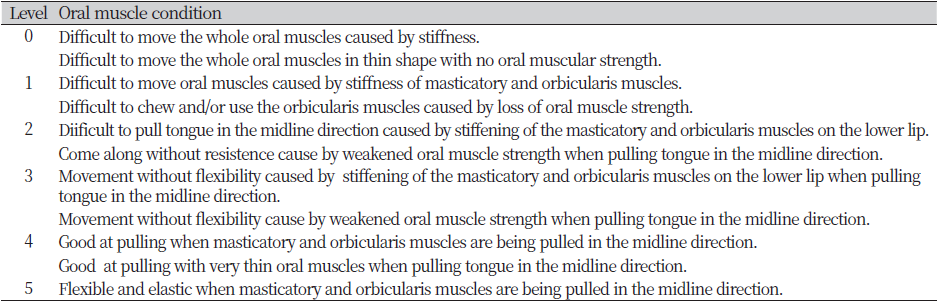
The oral hygiene intervention activities included oral observation, oral massage, oral hygiene management, and oral muscle training. The details of the activities are shown in <Fig. 3>. The “Jeong Min-Sook intraoral and extraoral massage” (mouth muscle massage) involves massaging while holding both intraoral and extraoral muscles to enhance oral muscle elasticity and flexibility. Intra-oral massage that does not involve holding onto both intraoral and extraoral muscles simultaneously does not provide information about the elasticity of oral muscles. <Table 2> shows the classification of muscle elasticity.
Moreover, the videos provided by the Korean Association for Oral Health were shared with the patients to encourage their self-care, and a calendar for mouth stretching exercises was sent to each household. In addition, the oral hygiene products used by the professionals for oral hygiene care were left at the participants’ homes so that the participants could continue to use them.
3. Halitosis measurement using a halitosis meter
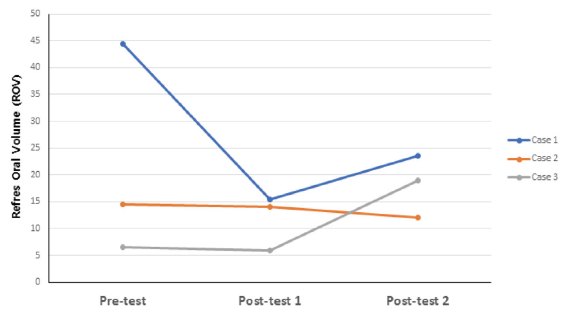
Changes in concentration of VSCs were determined using a halitosis meter (REFRES SX-105, ADONIS Electronics Corp, Japan) <Fig. 4>. Gas concentrations were measured on a scale of 0–200 ppm H2 gas, expressed as 0 to 100 Refres Oral Volume (ROV). Halitosis was measured as specified in the manufacturer's manual. The measurements were taken in oral mode. After the device beeped following a 30-second countdown, the participant bit down on the probe for 5 s until halitosis was measured. The halitosis severity was assessed based on the measurement results as follows: “no halitosis detected (≤30 ROV),” “slight halitosis detected (31–50 ROV),” “halitosis detected all the time (indicated for treatment) (51–70 ROV),” “definite halitosis detected (indicated for treatment) (71-90 ROV),” and “strong halitosis detected (indicated for treatment) (91–100 ROV).” The average of the two measurements was used to obtain accurate results.
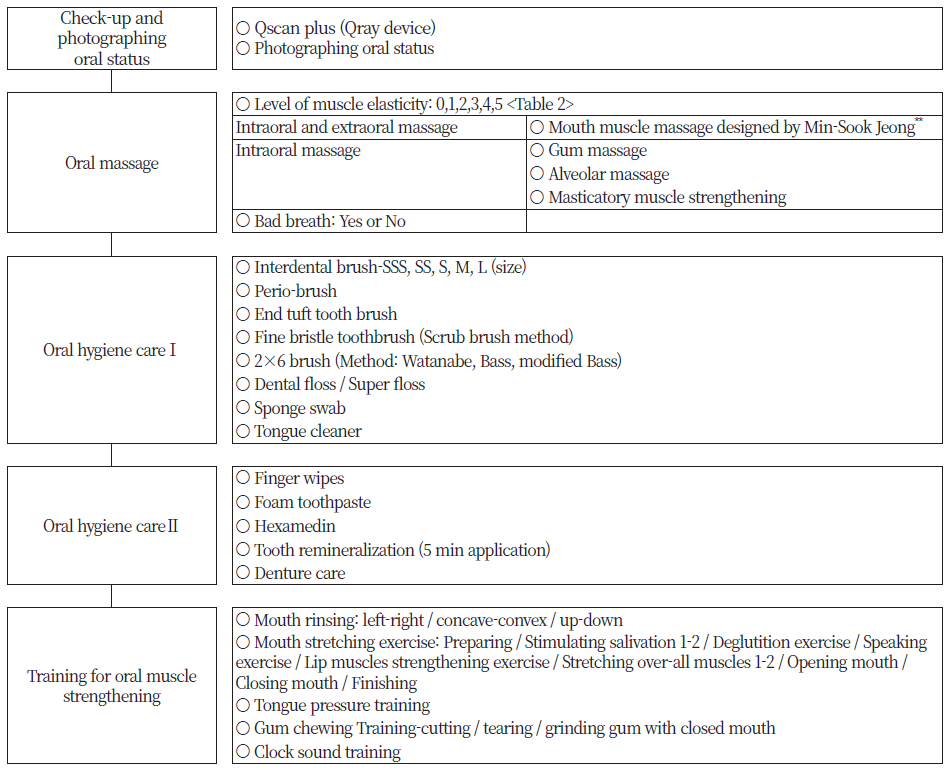
Fig. 3. Activities and/or related materials for visiting oral hygiene care intervention **Mouth muscle massage designed by Min-Sook Jeong: For this information, please refer to the following url. (https://www.youtube.com/watch?v=9vcu5sNuEuk YouTube Video provided by Korea Association for Oral Health)
4. Changes in oral health after oral hygiene interventions
1) Case 1
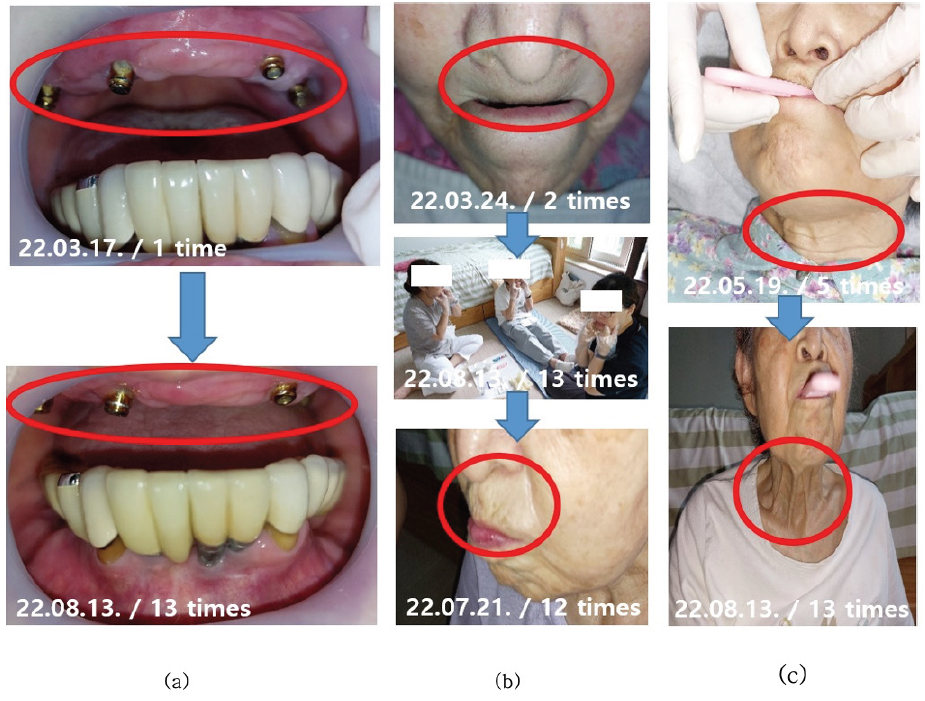
The case was a 91-year-old woman who overcame discomfort from xerostomia and halitosis <Fig. 5>. The patient wore a maxillary overdenture and had dental implants for all mandibular teeth except for her canine. She wore her dentures all day because when she removed her dentures for sleep, her upper lip curled into her oral cavity, leaving her mouth open and causing xerostomia and bad breath. Additionally, she wanted to replace her dentures due to gum swelling and pain caused by poor oral hygiene. The patient stated that she visited a dentist regularly but has never been educated on how to maintain and manage her dentures. She used a Waterpik in addition to a toothbrush, but poor oral hygiene had caused serious inflammation around the locator attachment and peri-implantitis. In addition, the patient’s saliva testing showed a high concentration of Porphyromonas gingivalis, a major pathogen of halitosis and acute and chronic periodontitis.
The intervention team recommended that the patient remove the dentures when going to sleep to ease gingival pain and to wear a mask to alleviate xerostomia and halitosis caused by removing the dentures.
Before the intervention, the patient had a muscle elasticity score of 2 (flexible, but not elastic), which increased to 3.5 after the oral hygiene intervention, indicating increased elasticity of the lip and cheek muscles. Before the intervention, the patient had severe xerostomia to the point of her lips sticking to her gums; however, weekly intraoral and extraoral massage using Dry Mund Gel, mouth stretching exercises, and tongue pressure training increased the salivary secretion, moistened the oral mucosa and tongue, firmed up the gums, and reduced gingival crevicular fluid. In addition, professional oral hygiene care around the dental implants using a toothbrush, interdental brush, and periobrush (periodontal brush) improved gingival health so that the gingival bleeding stopped. The patient’s caregivers also participated in the education and routinely performed oral hygiene care and intraoral and extraoral massages with the participant. <Fig. 6> shows the changes in halitosis. The patient had a high level of halitosis at baseline, at 44.5 ROV, which dropped to 15.5 ROV (no halitosis detected), at post-test 1, showing a dramatic decline in halitosis severity. In addition, while the patient had wanted to refabricate her dentures due to discomfort before the intervention, after the intervention, the patient was told by her dentist that her gingival conditions had improved substantially so that she no longer needed new dentures. The patient expressed her gratitude to the oral health care team for this.
2) Case 2
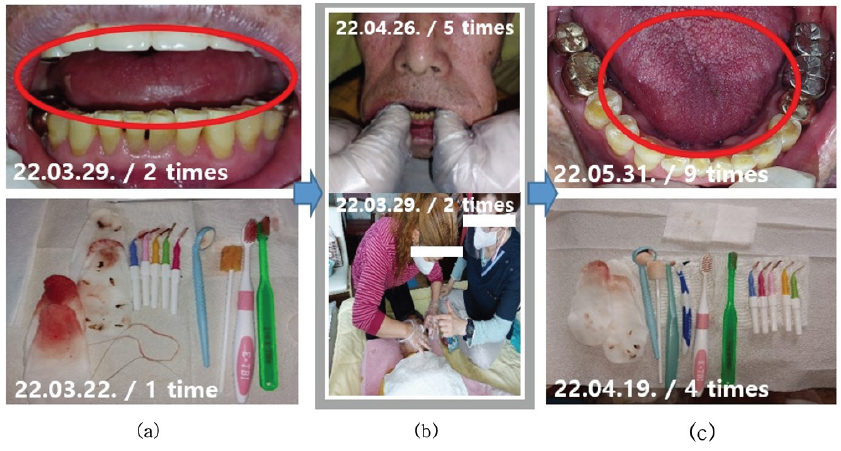
The case was a 76-year-old man who has received the home oral care service for 3 years as of the baseline examination and was chair-bound due to hemiplegia caused by cerebral infarction <Fig. 7>. The patient showed severe mouth breathing due to his inability to close his lips, which resulted in protrusion of the upper anterior teeth and diminished breathing sounds. Although the patient had been practicing oral hygiene by brushing his teeth on his own, there was often a significant amount of food debris in his mouth at each visit and he had significant gingival bleeding and pain even with manual intraoral and extraoral massages. Furthermore, supragingival calculus was detected in all teeth, and the teeth were overall mobile. Hence, the oral health care team checked for tooth mobility before starting each intervention activity and informed the caregiver about the possibility of tooth extraction. The lower right first molar was eventually extracted midway through the intervention. After providing specialized oral hygiene care and education, the patient’s muscle elasticity increased from 1 to 3 points. Muscle relaxation improved, and stippling was found on the attached gingiva surface, indicating a healthy gingival status. The patient had complained of pain and had significant gum bleeding even with manual oral massage before the intervention, but his gingival state improved markedly along with high salivary viscosity. After removing the mandibular anterior supragingival calculus using a hand scaler, the patient’s halitosis rapidly decreased, and the continued oral hygiene care education for the caregiver resulted in a noticeable decline in food debris in the oral cavity of the patient at 3 weeks into the education, which also contributed to the reduced halitosis. At 9 weeks (post-test 1), the patient could close his lips and breathe through his nose, unlike before. His halitosis value was 14.5 ROV and further dropped to 12 ROV on the final week of the intervention (week 12) <Fig. 6>. The saliva test still showed Porphyromonas gingivalis, which induces halitosis, but the number of pathogenic bacteria was reduced through the home oral care intervention, presumably the intraoral and extraoral massage and gum massage.
3) Case 3
The case was an 87-year-old man who was chair-bound due to hemiplegia and who had severe xerostomia from mouth breathing and consequent curled tongue <Fig. 8>. The tongue was straightened and the halitosis was reduced after the intervention. The patient had several general diseases, including hypertension, chronic lung disease, myocardial infarction, asthma, arthritis, cerebral infarction, kidney disease, and hyperlipidemia, and was taking 11 medications simultaneously. The patient showed reduced tongue muscle mass; the consequent tongue weight hindered mouth closing, which led to serious mouth breathing. The patient’s child, who works as the patient’s caregiver, assisted with oral care, but severe halitosis occurred due to interdental food debris and gum bleeding. After 12 weeks of professional oral hygiene care, the patient’s muscle elasticity increased from 2 to 3 points, the previously dry tongue straightened, and the phlegm attached to the soft palate was removed, leading to more relaxed breathing sounds. In addition, oral muscle massage to stimulate the parotid gland by pulling the masticatory muscle increased saliva production, and gum and alveolar ridge massage stimulated the bottom part of the tongue and, consequently, the submandibular gland and sublingual gland to alleviate the xerostomia. As a result of strengthened buccinator muscle, food residue in the oral cavity was nearly eliminated. The caregiver was also provided with intensive oral hygiene education. The patient’s oral hygiene was significantly improved after the caregiver assisted with oral care using tools such as sponge swabs (oral hygiene sponge) and finger wetty (finger wipes). The patient’s gingival swelling and bleeding decreased considerably, and the halitosis measurements remained similar at post-test 1 (week 9) at around 6 ROV (compared to 6.5 ROV at the baseline) <Fig. 6>, showing prevention of halitosis exacerbation through community care. However, the halitosis level rose dramatically to 19 ROV at post-test 2. In the saliva test, the patient had a ‘high’ risk for oral and systemic diseases before the intervention, which improved to ‘good health’ after professional oral care and education. However, at the last visit (week 12), the patient again showed a high concentration of pathogenic halitosis-inducing bacteria with a ‘very high’ risk for oral and systemic diseases. This is attributed to poor oral hygiene compliance during the short period in which home oral care intervention was paused due to the patient’s COVID-19 diagnosis and hospital appointment schedules. The 11 medications the patient was taking were also presumed to have adversely impacted his oral health. Continuous home oral care services were essential to improving the patient’s oral hygiene, and the oral hygiene education provided to the caregiver, as well as professional oral hygiene care services, had a grave impact on the patient’s oral hygiene status.
Discussion
The community care project was launched as a pilot project in 2019 by the Korean government. Most of the target population displays poor oral health, as they suffer from systemic disease and had difficulties practicing oral care without professional assistance [12]. Oral hygiene care using oral hygiene products and routine dental visits contribute to improving oral health, and whole-body and emotional health resulting from reduced halitosis enhances the quality of life of older adults [14]. Although oral care and health education have been limited due to the global coronavirus disease 2019 (COVID-19) pandemic, Cheonan-si was able to continue implementing the community care project owing to its home-based nature. Hence, professionals continued to provide oral care and education for older adults while adhering to basic infection control measures, such as the use of a face mask and ensuring adequate ventilation and disinfection [12]. The participants displayed high satisfaction not only with the home health care services but also with individualized professional oral hygiene services offered through the home oral health intervention program.
In case 1 of our study, xerostomia, the major cause of halitosis, was alleviated through oral hygiene care and education, intraoral and extraoral massage, mouth stretching exercises, and tongue pressure training. The patients in case 2 and 3 were chair-bound and displayed mouth breathing; hence, they could not perform oral hygiene without assistance. Thus, their caregivers were intensively educated in oral hygiene and trained to perform mouth stretching exercises at each intervention session. The caregivers were also educated on how to use sponge swabs (oral hygiene sponge) and finger wetty (finger wipe), which are products that can easily be used by non-professionals. The patient in case 2 showed decreased halitosis after the intervention. However, while the patient in case 3 showed a marked decline in halitosis on week 9, a dramatic increase was observed on week 12. We suspect that the patient’s long-term polypharmacy (>10 prescription drugs) as a result of various systemic diseases contributed to dry mouth [15].
Most community-dwelling older adults will face challenges in independent oral hygiene care as their physical functions deteriorate with aging [16]. Masticatory functions decline because of tooth loss and masticatory muscle atrophy, and deteriorating oral functions lead to general health problems [15,17]. Xerostomia, caused by polypharmacy due to various comorbidities and mouth breathing, is a major oral condition affecting older adults aged 65 years and over [15]. Reduced saliva secretion and poor oral hygiene cause bacterial proliferation and consequent halitosis [16,18], and severe halitosis has a toll on the individual’s interpersonal and social interactions and may even induce social phobia in serious cases [19].
In a study on older adults, Kim [20] reported that diminished physical activity due to COVID-19 and consequent depression leads to mental health issues such as cognitive impairment, dementia, and suicide. In their study on community-dwelling older adults, Joung et al. [8] reported that while older adults perceived the importance of oral health, they showed poor oral health due to factors such as discomfort caused by treatment procedures and high cost, in addition to higher levels of halitosis (55.82 ROV) compared to the normal levels. Son et al. [21] highlighted the need for education and institutional support to increase awareness of the importance of oral health care and oral hygiene practices to ensure that older adults continue to live healthy lives in their own homes. Previous studies have shown positive outcomes in terms of xerostomia and halitosis-the two most common oral health problems observed among older adults-after implementing oral exercise programs using mouth-stretching videos and posters [14,22].
In the present study, we observed reductions in halitosis after providing professional oral hygiene care along with oral muscle training, such as mouth rinsing, mouth stretching exercises, tongue pressure training, gum chewing training, and clock sound training, to older adults eligible for the community care project in Cheonan-si. Based on our case series, we recommend the following to prevent mental health issues arising from halitosis and to enhance patient quality of life.
First, patients who require oral hygiene care by caregivers and personal care assistance, such as chair-bound and bedridden older adults, should be highlighted as individuals requiring intensive oral care and be provided intensive and more frequent care services. Second, there is a need to develop and implement individualized home oral care programs that are tailored to the oral status and needs of older adults suffering from systemic diseases. Third, a sufficient number of dental hygienists is needed to ensure that community care recipients continue to receive oral health care services, and a professional curriculum should be devised to foster the competencies required for providing relevant interventions. Fourth, work guidance and standard operating procedures should be established to systematize the implementation of community care policies nationwide, and a continuous, integrated, and tailored management system should be devised. Fifth, to keep abreast of technological advances in artificial intelligence (AI), mobile oral care applications utilizing AI-based instruments and platforms should be developed to better engage older adults and their caregivers in oral health care.
This study has several limitations. First, we aimed to provide home intervention services once every week; however, the home visit schedules were inconsistent for some patients due to reasons such as COVID-19 diagnosis, emergency hospitalization, medical examination schedules, and other personal situations, which hindered measuring changes in halitosis across time points. Second, the time of halitosis measurement was inconsistent, as visiting the patients at the same time every week was challenging. Furthermore, the oral environmental factors (e.g., meal status, toothbrushing status) at the time of halitosis measurement might have differed, limiting the generalizability of the results.
Despite these limitations, this study is significant in that we directly observed and assessed changes in the oral health status of older adults with halitosis while providing home oral care interventions as part of the community care project. Moreover, the reduction of halitosis achieved through a 12-week program including oral hygiene care and oral muscle training increased the satisfaction of both the patients and their caregivers.
Future studies should conduct focus group interviews to explore the essential factors for promoting the community care project and analyze the differences in participant satisfaction with home oral care intervention programs depending on their baseline oral status. In addition, randomized controlled trials and longitudinal studies with long-term follow-ups are also necessary to validate the effectiveness of the oral health interventions observed in case studies.
Conclusions
Home oral care services contributed to improving oral health and reducing discomfort from halitosis among older adults with halitosis, thereby enhancing their perceived quality of life.
1. In addition to professional oral hygiene care, oral muscle training such as mouth rinsing, mouth stretching exercises, tongue pressure training, gum chewing training, and clock sound training, led to positive changes in halitosis.
2. In case 1, the concentration of VSCs was 44.5 ROV before the intervention but dropped dramatically to the point of no halitosis detected (15.5 ROV) at post-test 1.
3. In case 2 (a chair-bound patient), the halitosis decreased from 14.5 ROV at baseline to 12 ROV after the intervention.
4. In case 3, halitosis remained from 6.5 ROV at the baseline to 6 ROV on week 9, but markedly rose on week 12, suggesting that oral health is very linked to systemic disease.
Therefore, this home oral care intervention was effective in preventing halitosis and improving oral health. The findings of this study underscore the need for individualized home oral care programs tailored to the specific characteristics of older adults with various systemic diseases in addition to halitosis to ensure systematic administration of these interventions.