Introduction
Development of the modern society and advancements in medical technologies have improved the living conditions and extended the human life expectancy. In 2020, 15.7% of the total population in Korea was aged above 65 years [1]. The rapid increase in the proportion of the elderly population has highlighted the importance of health problems and the quality of life of the elderly. In particular, oral health problems are closely related to dietary habits and are an essential factor for maintaining a healthy life [2].
With the growing aging population and the growing demand and demand for dentures known as ‘second teeth’, starting in July 2012, full denture benefits have begun to be offered to seniors aged 75 and over in South Korea. In July 2016, the age cutoff for availing this benefit was lowered to 65 years, thus further expanding the scope of health insurance coverage for dentures. In a 2018 survey, it was found that approximately 4 million elderly wore dentures. Hence, oral hygiene and appropriate management of dentures are important to maintain restored oral health for a prolonged period [3]. However, Moskona and Kaplan [4] reported that only 16.7% of denture wearers clean their dentures properly. Moreover, Jagger and Harrison [5] reported that some old adults have difficulties in cleaning the dentures and wear unhygienic dentures.
Two methods are commonly used for cleaning dentures: physical and chemical. Physical cleaning methods include washing under running water, cleaning with salt or toothpaste, soap, or ultrasonic cleanser [6]. In a previous study on the methods of denture cleaning in Korea, 33.6% of the elderly reported using a toothpaste with brush for cleaning, while 24.8% washed their dentures under running cold water [7]. Heath et al. [8] reported that brushing with water does not effectively remove the discoloration and organic residues on the dentures and recommended using toothpaste with low abrasion to clean the dentures adequately. Chemical cleaning methods include using commercially available disinfecting pill products or soaking in chlorhexidine solution [9,10]. However, Hwang and Shin [11] contended that the chemical cleaning methods cannot completely replace the effects of brushing in removing the foreign substances.
In general, toothpaste for cleaning the tooth surface contains abrasive ingredients that can abrade and scratch the surface of dentures, which are softer than natural teeth [12]. In a previous study, brushing the surface of self-curing denture base resin with toothpaste increased the roughness compared to brushing with soap, disinfecting pill, mouthwash, and ethanol [12]. Microorganisms can deposit in these rough surfaces; therefore, care is necessary [13].
To date, there is no toothpaste available in Korea for cleaning dentures, and there are no clearly established standards. Therefore, this study evaluated the depth of abrasion and the morphological changes in the dentures after using liquid-type non-abrasive denture cleanser (NAC) with no abrasive ingredients and enhanced cleaning power with vegetable surfactants to provide basic data about the selection and use of denture cleaners.
Methods
1. Materials
Self-curing denture base resins (ProBase cold, Ivoclar vivadent, Schaan, Fürstentum Liechtenstein) were mixed according to the manufacturer’s instructions and placed in a rectangular Teflon mold (15 mm×8 mm×7 mm) to create resin blocks. The surface of the resins was polished step-by-step to 1,200 grit using sandpapers (Allied high-tech products, Rancho Dominguez, CA, USA). The resin specimen was cleaned and stored in a humidifier (Dry keeper C-3W, Sanplatec Corp., Osaka, Japan) for complete drying. The weight of the resin specimen was measured for 3 days, every 24 hours, using an electronic scale (PAG214, OHAUS corporation, USA) with a measurement range of 10-4 to 210 g. When the difference in weight compared to the previous measurement was less than 0.001 g, the weight was set as the baseline weight (W0[g]). The types of cleaning agents that were evaluated included distilled water (DW), NAC (Dr. Choi’s Toothpaste Care, Dr. Choi’s KOREA Co., Ltd., Seoul, Korea), toothpaste (TP, Perio Cavity Care, LG Household & Health, Daejeon, Korea). A total of 30 specimens were assigned to each group.
2. Methods
An automatic toothbrushing machine (V8 Cross brushing machine, Sabri Co., USA) with a back-and-forth motion was used for brushing. Toothpaste was mounted on a toothbrush (Butler GUM Classic toothbrush #211, Sunstar Americas, Inc., Chicago, IL, USA) for 200 g of total weight. DW and NAC, which are in liquid form, were placed in the chamber as such. TP was placed in the chamber in the form of a slurry in which TP and DW were mixed in a ratio of 1:3. One specimen was installed in each chamber, and the chamber was filled so that the specimen was completely immersed. A total of 10,000 counts of brushing, which is equivalent to brushing per year, was performed on the dentures, and abrasion of the resin specimen was measured 1,000 times for each toothpaste [14]. Each specimen was tested under the same conditions, and the liquid and toothbrush were changed every time the specimen was changed. After brushing was completed, the specimen was cleaned and dried in a humidistat. The weight was measured in the same manner as that for W0, and the 10,000th weight was recorded as W10(g). The thickness of the abraded specimen (TL) was calculated using the following equation [8,15].
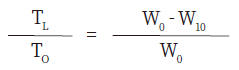
TO = Initial thickness of the specimen (mm)
TL = Thickness of the abrasion (mm)
W0 = Thickness of the abraded specimen (g)
W10 = Dried weight of the abraded specimen (g)
One resin specimen was randomly selected from each group, and the surface of the specimen after brushing was evaluated using field emission scanning electron microscopy (FE SEM-S800; Hitachi, Tokyo, Japan). Each specimen was completely dried and coated with a gold sputter, to be observed at 100×.
3. Statistical analyses
Shapiro-Wilk normality test was performed to confirm that the normality of data was satisfied. The differences in mean TL for each type of cleanser and the counts of brushing were assessed using one-way ANOVA and Tukey’s post hoc analysis. SPSS 23.0 (IBM Co., Armonk, NY, USA) was used for all statistical analysis, and p<0.05 were considered statistically significant.
Results
1. Abrasion according to the type of denture cleaner and count of brushing
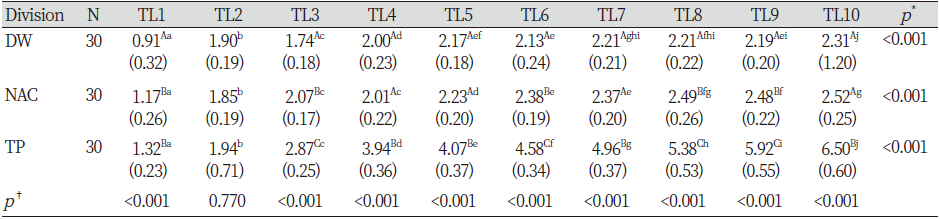
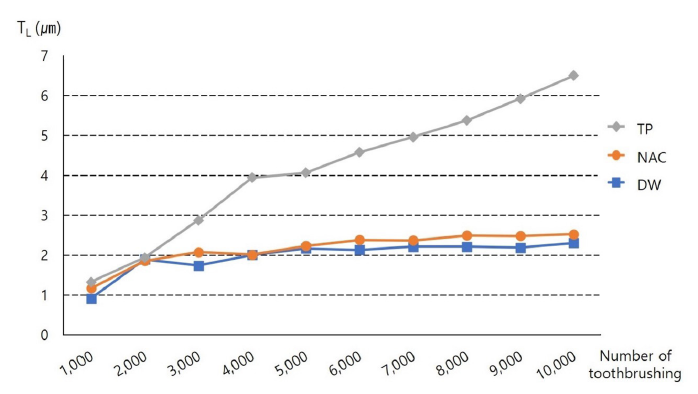
The composition of the cleansers used in each group is shown in <Table 1>, and the TL trend according to the count of brushing in each group is illustrated in <Fig. 1>. TL after the 1,000th brushing was not significantly different between the NAC and TP groups. However, TL after the 10,000th brushing was approximately 3 times higher in the TP group than in the DW and NAC groups, and there was no difference in TL between the DW and NAC groups (p> 0.05). In all the three groups, the TL was significantly different between the 1,000th and 10,000th brushing (p<0.001). In the DW and NAC groups, TL was sometimes showed no significant change as the count of brushing increased (p> 0.05). However, TL showed a significant change between the 1,000th and 10,000th brushing in the TP group (p<0.05) <Table 2>.
Table 1. Raw material information by denture cleanser group
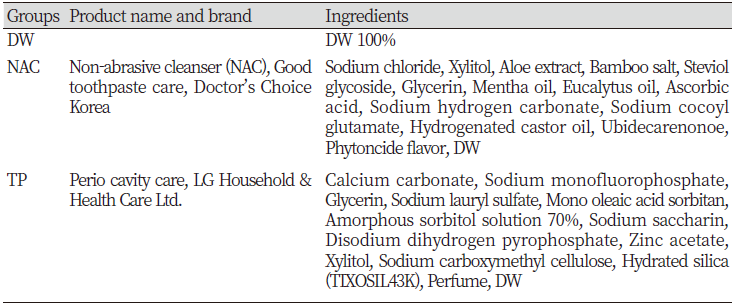
|
|
DW is distilled water. NAC is non-abrasive cleanser. TP is toothpaste. |
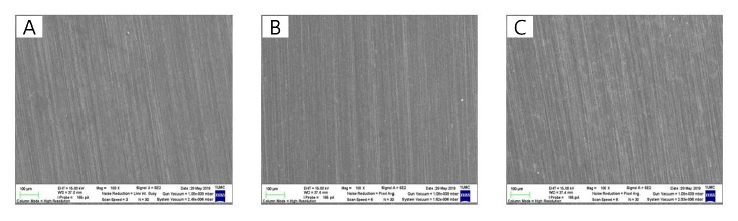
2. Morphological assessment of the tooth surface
The specimen surface was assessed with SEM after the 10,000th brushing. Regular dents were observed in all specimens in the direction the toothbrush moved, and the surface of the TP group was rougher than that of the DW and NAC groups <Fig. 2>.
Discussion
Prolonged use of unhygienic dentures can cause serious oral health problems such as stomatitis, gingivitis, bad breath, and opportunistic fungal infections [8,16-19]. In particular, bacteria such as Candida albicans can adhere to the surfaces of resins of the dentures and proliferate [16]. Candida carrier rates were 70% and 39%, respectively, with and without dentures, which was a statistically significant difference [20]. This can cause oral health issues, pneumonia, and infections of the other body organs, as well as systemic diseases such as a 4-times higher prevalence of cancer in the elderly with reduced immunity. Therefore, the cleanliness of the dentures must be maintained [8,17-19]. Removing the plaques from dentures and maintaining their hygiene is essential to prevent the other complications mentioned above [21]. However, the elderly might be unable to clean the dentures appropriately due to reasons such as decreased vision caused by aging, inadequate hand movements, and discomfort in walking [22]. In particular, the condition of the dentures of the elderly who are not interested in denture management or who have learned wrong information is inevitably poor. Therefore, simple methods and safe cleansers that can effectively remove the foreign substances and bacterial plaque on dentures without damaging them and affecting oral health would be necessary.
In this study, abrasions on dentures after cleaning with NAC was assessed. After 10,000 brushings, abrasion of the resin specimen in the NAC group (2.52±0.25 µm) was 1/3 of that in the TP group (6.50±0.60 µm), while it was similar to that in the DW group (2.31±1.20 µm). Park et al. [15] reported that the average abrasion caused by soap solution and toothpaste was 2.46 µm and 13.85 µm, respectively, after 20,000 brushings. The frequency of abrasion caused by toothpaste was 5 times higher than that by the soap solution, which is consistent with our findings. Additionally, similar to our finding, previous studies reported that the decrease in weight of the resin specimen was approximately 5 times higher after brushing with toothpaste for 300 minutes compared to that by brushing with distilled water [23].
SEM was used to evaluate the surfaces of dentures, which revealed that the surface in the TP was rougher than in the other two groups. This is consistent with the finding of a previous study, which confirmed that brushing the denture resin with toothpaste leads to a rough surface compared to that by brushing with soap solution [12]. Moreover, our finding confirms that brushing the dentures with commercially available toothpaste leads to increased roughness of the surface than brushing with distilled water [24].
Tellefsen et al. [25] reported that brushing the dentures with toothpaste results in a high degree of abrasion of the denture surface, even when the force applied during brushing is weak. In other words, irrespective of the force applied during brushing, scratches are induced by the abrasive ingredients of toothpaste, and this can lead to the colonization of bacteria [13,25]. The main factors that affect the abrasion of the dental base resin are the size and hardness of abrasive materials in the cleansers and the intensity and speed of brushing [26]. Several previous studies on denture deformation and bacterial growth caused due to the abrasive material of toothpaste recommend using detergent for dentures or dish soap as the cleanser [27,28]. NAC evaluated in our study did not contain any abrasive materials and caused similar abrasion of the denture base resin as DW. Therefore, it is thought that NAC can be used as a new denture cleanser.
In all three groups, TL significantly changed from the 1,000th to 10,000th brushing (p<0.001), and it is thought that the abrasion was inevitably caused by the physical motion of the toothbrush. Therefore, a soft denture brush or toothbrush for physical cleaning must be selected to minimize the damage to the denture surface [29].
In this study, abrasion caused by NACs was assessed. In future studies, the antibacterial effects and cytotoxicity of denture cleansers should also be assessed. Additionally, the cleansers should be tested on actual denture wearers to support the clinical studies for efficacy, safety, and evaluation of patient satisfaction.
Conclusions
This study aimed to provide basic data about the selection and use of denture cleansers by evaluating the abrasion on denture base resins after using NAC. The following conclusions were made based on the results. The average TL after brushing was 2.31±1.20 µm, 2.52±0.25 µm, and 6.50±0.60 µm in the DW, NAC, and TC groups, respectively. The average TL was not significantly different between the DW and NAC groups (p> 0.05). However, the TL was significantly greater in the TC group than in the two other groups (p<0.001). The surface roughness was assessed using SEM, which demonstrated that the specimen of the TC group was rougher than that of DW and NAC groups. Based on these findings, toothpaste is not recommended to maintain the longevity of dentures and for oral health, and NACs would be ideal for cleaning the dentures.