1Department of Dental Hygiene, Shinhan University
2St. Hugh Hospital, Speech Therapy Lab
Correspondence to Kyeong-Jin Lee, Department of Dental Hygiene, Shinhan University, 95 Hoam-ro, Uijeongbu-si, Gyeonggi-do, 11644, Korea. Tel: +82-31-870-3450, +82-10-2889-6484, Fax: +82-31-870-3459, E-mail: white2783@naver.com
Volume 24, Number 3, Pages 209-18, June 2024.
J Korean Soc Dent Hyg 2024;24(3):209-18. https://doi.org/10.13065/jksdh.20240302
Received on May 07, 2024 , Revised on May 16, 2024, Accepted on May 22, 2024, Published on June 30, 2024.
Copyright © 2024 Journal of Korean Society of Dental Hygiene.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License(http://creativecommons.org/licenses/by-nc/4.0)
Objectives: This study aimed to develop educational content for a smartphone app on oral muscle training and examine its effects on the elderly population. Methods: A total of twelve training sessions were delivered through the smartphone app over a six-week period, from late August to early October 2023. Each session lasted approximately 60 minutes. Participants were followed up after the program. Results: The experimental group showed significant improvements in oral health before and after using the smartphone app. These improvements included decreased dental plaque (p<0.05) by 0.69 units, decreased gingivitis (p<0.001) by 0.99 units, decreased tongue plaque (p<0.01) by 1.11 units, increased salivary secretion rate (p<0.001) by 0.73 units, increased hard palate strength (p<0.001) by 5.25 units, and increased soft palate strength (p<0.01) by 6.82 units. Compared to the control group, the experimental group showed significant improvements in dental plaque (p<0.001), gingivitis (p<0.001), and tongue coating (p<0.01). Conclusions: This study found that oral muscle strengthening training using the smartphone app effectively improved oral health in the elderly. The developed app content has the potential to be a valuable tool for promoting oral health in this population within their daily routines. However, further efforts are needed to ensure clear communication and effective utilization of the training program through user training or educational materials.
Aged, Muscle strength, Oral health, Smartphone
The modern world has seen a surge in information and communication technologies (ICTs) like computers, the internet, and smartphones. These technologies have diversified the ways we acquire information and education. Notably, smartphones are gaining popularity among older adults, emerging as a tool for enhancing social participation, improving daily satisfaction, and boosting quality of life. Research suggests a positive correlation between smartphone use and life satisfaction in older adults [1]. Additionally, access to ICTs has been linked to improved psychological well-being in this population [2]. By providing diverse training in smartphone use, we can help older adults adapt to a changing society and bridge the information gap that can contribute to inequality [3]. A study comparing life satisfaction among older adults with and without smartphone education found that those with training reported higher satisfaction levels [2]. Similarly, a 2017 study by Shin and Kwon [4] demonstrated that older adults’ self-efficacy increased after participating in a communication program (SNS activity) that involved using smartphones for social networking activities with friends.
Effective health behavior change hinges on individual recognition of the need for modification [5]. This trend extends to oral health education, where there is a growing demand for smart media interventions. This increasing smartphone use among older adults presents a unique opportunity. Developing smartphone-based oral health educational content that is accessible anytime, anywhere can significantly enhance educational effectiveness for this population [6].
Aging often leads to a decline in oral health due to weakened oral muscles and diminished functions like mastication, swallowing, and articulation [7]. Reduced mastication can limit food intake, lead to digestive problems, and even cause social anxiety due to embarrassment about eating in public [8]. Oral muscles play a critical role in supporting occlusal and oral motor functions like mastication, articulation, and swallowing. Maintaining proper oral function relies heavily on strong oral muscles [9]. A 2004 Japanese study demonstrated the effectiveness of a combined geriatric oral health program and exercise program to improve oral health in older adults [10]. Tongue resistance training is being explored as a treatment strategy to prevent dysphagia caused by weakened tongue muscles in older adults and those with age-related impairments [11]. Research also shows that oral muscle exercise programs can significantly improve mastication, swallowing, and saliva production [12]. Therefore, strengthening oral muscles is essential for improving oral health and the quality of life of older adults.
However, current oral muscle exercise programs for older adults are primarily offered through educational institutions or public facilities, limiting participation for those with mobility challenges or low social engagement. Additionally, research in this area remains scarce. In light of these limitations, this study aimed and evaluate smartphone-based educational content for oral muscle strength training specifically designed for older adults. Our ultimate goal is to promote better oral health among this population.
This study employed a posttest-only equivalent control group design. Participants were randomized into an experimental group and a control group to investigate the effectiveness of smartphone-based oral muscle strength training. The study was approved by the Institutional Review Board of Shinhan University (IRB approval no: SHIRB-202403-HR-225-02).
Participants were recruited from senior welfare centers in the Seoul metropolitan area using non-probability sampling methods. We included individuals aged 65 and over who were able to communicate effectively, had sufficient mobility, owned a personal cell phone, and could access content using simple gestures. All participants provided informed consent to participate in the study.
The sample size was determined based on a previous study [13] using the G*power 3.1.9.4 software. With a significance level of 0.05, an effect size of 0.8, and a power of 0.8 [14], the minimum sample size was calculated to be 42, with 21 participants in each group. To account for potential dropouts, we initially enrolled 60 participants (30 per group). After excluding those who failed to complete the 12-week intervention or withdrew from the study, the final analysis included data from 28 participants in the experimental group and 23 in the control group <Fig. 1>.
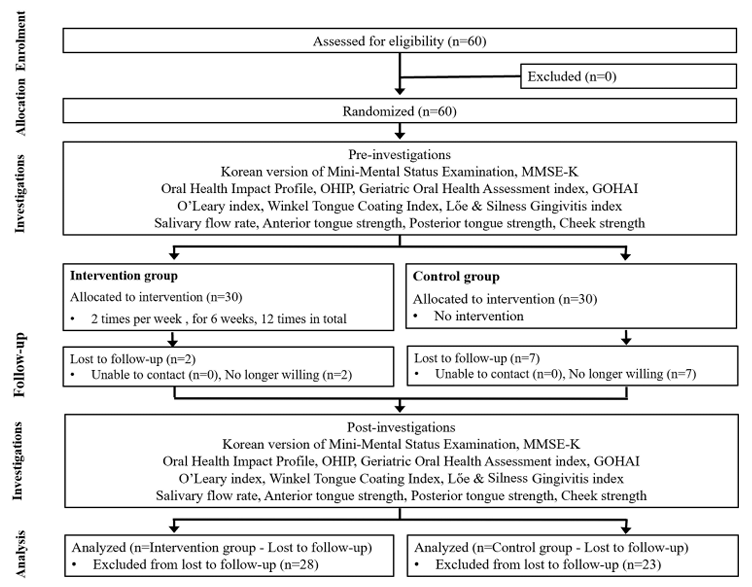
Fig. 1. Selection procedures of research subjects
The developed educational content for oral strength training included pronunciation training, tongue exercise games, and six instructional videos <Fig. 2>. These videos covered pre-meal mouth stretching, lip exercises, general mouth exercises, gum massage, salivary gland massage, and tongue exercises.
Participants received a total of 12 smartphone-based training sessions over a six-week period from late August 2023 to early October 2023. The sessions, lasting approximately 60 minutes each, were conducted at the participants’ affiliated facilities.
To ensure user comfort, the researcher downloaded the app with each participant before the program began and provided personalized training on its functionality. During the intervention period, participants learned independently using the embedded exercise videos and game content within the app.
The study employed a pre-test and post-test design. The pre-test was conducted one week before the training program, and the post-test was conducted three days after program completion. Two different researchers independently performed oral examinations and oral muscle strength measurements before and after the program.
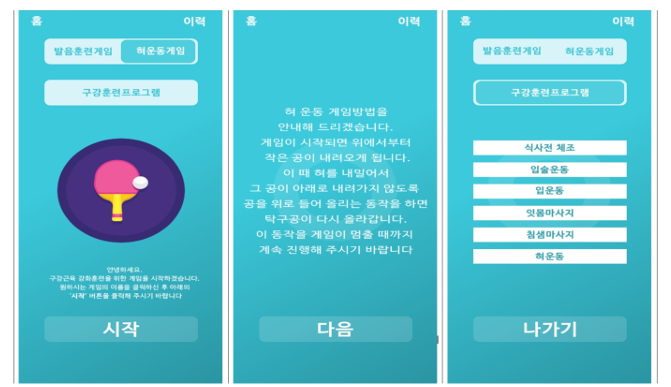
Fig. 2. Main screen of the smartphone app for oral muscle strength training
Participant characteristics were assessed using a self-administered questionnaire, including demographics (sex, age, education level, economic status, spousal cohabitation status, and cognitive function using the Korean version of the Mini-Mental Status Examination [MMSE-K]) [15]. The MMSE-K assesses seven domains, including attention, calculation, registration, recall, language, visual orientation, and time/place orientation. A score of 24 or higher indicates normal cognitive function, with a maximum possible score of 30. Oral health behaviors were also evaluated, including toothbrushing frequency, tongue cleaning, gum cleaning, oral hygiene product use, toothpick use, and professional scaling within the past six months.
Oral health-related quality of life was measured using the Geriatric Oral Health Assessment Index (GOHAI) [16] and the Oral Health Impact Profile (OHIP) [17], with higher scores indicating poorer quality of life. Dental plaque was assessed using the O’Leary index [18], with lower scores indicating less bacterial plaque. Tongue coating was evaluated using the Winkel Tongue Coating Index [19], where a score of 0 indicates no coating and 1 indicates coating. Gingival inflammation was assessed using the Lὅe & Silness’ gingivitis index [20], where scores range from 0 (no inflammation) to 3 (severe inflammation). Given the potential for tooth loss in older adults, all teeth were included in the gingival inflammation assessment, with higher scores indicating greater severity.
Unstimulated salivary flow rate (SFR) was measured in grams (g) (1 mL = 1 g). Participants were instructed to swallow all saliva before collection, and then close their mouths for five minutes to allow saliva to pool. The pooled saliva was then expectorated into a test tube [21].
Oral muscle strength was assessed using the Iowa oral performance instrument (IOPI Medical, WA, USA) for anterior tongue strength (ATS), posterior tongue strength (PTS), and lip strength (LS) [22]. For ATS, the bulb was placed between the anterior tongue and the hard palate. PTS measurements were taken with the bulb between the posterior tongue and the hard palate/soft palate junction. Finally, LS was measured by placing the bulb between the inner aspect of the central incisors and the inside of the lateral lip. Participants were instructed to squeeze the bulb as hard as possible. Three measurements were taken for each muscle group, and the maximum value (kPa) was recorded according to the manufacturer’s recommendation.
Data were analyzed using IBM SPSS program (ver. 22.0; IBM Corp., Armonk, NY, USA) with a significance level of alpha = 0.05. Chi-square and Fisher’s exact test compared baseline characteristics (demographics and oral health behaviors) between groups. Independent t-tests assessed baseline homogeneity, while paired t-tests compared pre- and post-test results within each group. Finally, independent t-tests investigated post-test measurement differences between the groups.
Baseline characteristics of the participants, including sex, age, education, socioeconomic status, spousal cohabitation status, and MMSE-K scores showed no statistically significant differences between the experimental and control groups, confirming their homogeneity <Table 1>. The participant pool was skewed female, with the most common age range being 75-84 years old. Most participants had a high school education or higher, belonged to a lower socioeconomic bracket, and were widowed. The mean MMSE-K score was 25.82 for the experimental group and 26.17 for the control group <Table 1>.
Table 1. General characteristics of the participants
Unit: N(%)
| Characteristic | Division | Intervention group (N=28) | Control group (N=23) | Total (N=51) | p |
|---|---|---|---|---|---|
| Sex | Male | 2(7.1) | 2(8.7) | 4(7.8) | 0.617b |
| Female | 26(92.9) | 21(91.3) | 47(92.2) | ||
| Age (yr) | 65-74 | 9(32.1) | 9(39.1) | 18(35.3) | 0.091a |
| 75-84 | 17(60.8) | 8(34.8) | 25(49.0) | ||
| ≥85 | 2(7.1) | 6(26.1) | 8(15.7) | ||
| Education level | ≤Primary school | 10(35.7) | 8(34.8) | 18(35.3) | 0.691a |
| Middle school | 6(21.4) | 3(13.0) | 9(17.6) | ||
| ≥High school | 12(42.9) | 12(52.2) | 24(47.1) | ||
| Economic status | Upper | 2(7.1) | 6(26.1) | 8(15.7) | 0.165a |
| Middle | 12(42.9) | 9(39.1) | 21(41.2) | ||
| Low | 14(50.0) | 8(34.8) | 22(43.1) | ||
| Spouse | Widowed | 15(53.6) | 9(39.1) | 24(47.1) | 0.568a |
| Cohabitating | 9(32.1) | 9(39.1) | 18(35.3) | ||
| divorced | 4(14.3) | 5(21.8) | 9(17.6) | ||
| MMSE-K | 25.82±3.56 | 26.17±2.65 | 0.696c |
MMSE-K: Korean version of the Mini-Mental Status Examination
*by chi-square test, **by Fisher’s exact test, ***by independent t-test
Oral health behaviors, including toothbrushing frequency, tongue and gum cleaning, oral hygiene product use, toothpick use, and frequency of scaling in the past six months, were assessed. No statistically significant differences were found between the groups, confirming baseline homogeneity <Table 2>. Brushing teeth at least three times daily, consistent tongue and gum cleaning, and regular use of oral hygiene products were the most common practices in both groups. However, the experimental group had a higher percentage of participants who did not receive professional scaling within the last six months.
Table 2. Oral health-related behavior characteristics
Unit: N(%)
| Characteristics | Division | Groups | Total (N=51) | p | |
|---|---|---|---|---|---|
| Intervention group (N=28) | Control group (N=23) | ||||
| Number of times the patient brushed their teeth daily | 1 | 6(21.4) | 4(17.4) | 10(19.6) | 0.369* |
| 2 | 9(32.2) | 4(17.4) | 13(25.5) | ||
| ≥3 | 13(46.4) | 15(65.2) | 28(54.9) | ||
| Tongue cleaning | Always | 18(64.3) | 16(69.6) | 34(66.6) | 0.486* |
| Sometimes | 6(21.4) | 6(26.1) | 12(23.5) | ||
| I don’t do it | 4(14.3) | 1(4.3) | 5(9.9) | ||
| Gum cleaning | Always | 16(57.1) | 11(47.8) | 27(52.9) | 0.085* |
| Sometimes | 2(7.1) | 7(30.5) | 9(17.6) | ||
| I don’t do it | 10(35.7) | 5(21.7) | 15(29.5) | ||
| Use of oral hygiene products | Yes | 22(78.6) | 19(82.6) | 41(80.4) | 0.500** |
| No | 6(21.4) | 4(17.4) | 10(19.6) | ||
| Use of toothpicks | Yes | 14(50.0) | 7(30.4) | 21(41.2) | 0.130** |
| No | 14(50.0) | 16(69.6) | 30(58.8) | ||
| Scaling within the last months | Yes | 10(35.7) | 12(52.2) | 22(43.1) | 0.185** |
| No | 18(64.3) | 11(47.8) | 29(56.9) | ||
*by chi-square test, **by Fisher’s exact test
Following the program, the experimental group showed significant improvements in dental plaque (p<0.05), gingivitis (p<0.001), tongue coating (p<0.01), and salivation (p<0.001) compared to baseline measurements. Specifically, dental plaque decreased by 0.69 units, gingivitis decreased by 0.99 units, tongue coating decreased by 1.11 units, and salivation increased by 0.73 units <Table 3>. Post-hoc analysis revealed significantly lower levels of dental plaque (p<0.001), gingivitis (p<0.001), and tongue coating (p<0.05) in the experimental group compared to the control group <Table 3>.
Table 3. Effectiveness of the smartphone app program in promoting oral health
| Variables | Intervention group (N=28) | Control group (N=23) | p** | ||||
|---|---|---|---|---|---|---|---|
| Pre | Post | p* | Pre | Post | p* | ||
| OHIP-14 | 56.14±9.80 | 53.75±13.47 | 0.284 | 55.00±12.19 | 56.26±10.52 | 0.745 | 0.469 |
| GOHAI | 42.64±9.00 | 43.28±13.24 | 0.758 | 38.56±5.91 | 41.39±8.48 | 0.191 | 0.556 |
| O’Leary index | 1.60±0.95 | 0.91±1.01 | 0.039 | 2.19±1.55 | 2.30±1.01 | 0.805 | <0.001 |
| Löe & Silness index | 2.14±0.81 | 1.15±0.22 | <0.001 | 2.59±1.92 | 3.39±1.71 | 0.096 | <0.001 |
| Tongue coating | 2.79±1.66 | 1.68±1.18 | 0.001 | 3.57±1.80 | 2.87±2.07 | 0.312 | 0.020 |
| Saliva flow rate (g) | 1.07±0.67 | 3.40±0.64 | <0.001 | 1.55±1.55 | 1.53±0.87 | 0.944 | 0.324 |
OHIP-14: Oral Health Impact Profile, GOHAI: Geriatric Oral Health Assessment index
*by paired samples t-test
**by independent samples t-test
The intervention led to significant improvements in both ATS and PTS within the experimental group. Compared to baseline measurements, ATS increased by 5.25 units (p<0.001) and PTS increased by 6.82 units (p<0.01). However, post-hoc analysis revealed no significant difference in tongue strength between the experimental and control groups <Table 4>.
Table 4. Effectiveness of the smartphone app for oral muscle strengthening
| Variables | Intervention group (N=28) | Control group (N=23) | p** | ||||
|---|---|---|---|---|---|---|---|
| Pre | Post | p* | Pre | Post | p* | ||
| Anterior tongue strength (kPa) | 35.46±7.58 | 40.71±7.55 | <0.001 | 40.87±13.73 | 43.52±12.73 | 0.465 | 0.101 |
| Posterior tongue strength (kPa) | 35.61±12.63 | 42.43±9.87 | 0.001 | 41.61±14.29 | 37.57±12.35 | 0.300 | 0.124 |
| Cheek strength (kPa) | 21.64±8.33 | 24.82±6.57 | 0.069 | 26.48±11.29 | 24.61±6.87 | 0.483 | 0.911 |
*by paired samples t-test
**by independent samples t-test
The surge of mobile internet and innovative devices like smartphones, driven by advancements in ICT and internet access, has exposed a concerning trend: an age-related information gap [23]. This gap necessitates increased information literacy education for older adults who may be disadvantaged in utilizing technology. Smartphone-based education offers a convenient solution, potentially improving digital literacy and information access for this population. In light of this need, our study developed and evaluated the effectiveness of educational smartphone app content specifically designed for oral muscle-strengthening training in older adults.
While the subjective oral health-related quality of life measures (OHIP-14 and GOHAI) showed a trend towards improvement after the program, these changes were not statistically significant. This aligns with findings from a previous virtual-reality-based oral muscle training study [13]. Both OHIP-14 and GOHAI assess the level of discomfort or pain experienced due to oral health-related problems. The lack of significant improvements in these measures might be attributed to the relatively short six-week training period, potentially limiting participants’ perception of changes in their oral health. Future studies with longer intervention durations could provide further insights.
On the other hand, the program demonstrated significant reductions in dental plaque, gingivitis, and tongue coating, mirroring findings from a previous virtual reality study [13] and aligning with other research. Studies have shown that integrated oral exercise programs in older adults can lead to reduced bacterial plaque and gingivitis [24], with similar findings for reduced dental caries in middle-aged adults [25]. These results suggest that the oral exercises likely improved oral health by enhancing conditions within the mouth, such as saliva production. Additionally, the training may have heightened participants’ awareness of oral hygiene, potentially leading to improved oral hygiene practices.
This study observed a significant increase in salivation, aligning with findings from a previous virtual reality-based oral muscle training [13] and a 2020 tongue exercise program [26]. Saliva analysis is gaining traction not only for oral health assessment but also as a biomarker for systemic diseases and treatment monitoring [27]. These findings suggest that consistent oral strength training stimulates salivary glands, leading to increased saliva production. Research suggests that increased salivation improves oral function regardless of age, medication use, or dentures [28]. In this study, the observed improvement in oral hygiene (reduced plaque, gingivitis, and tongue coating) might be linked to increased salivation.
Oral muscle strength and masticatory function are highly correlated [29]. Therefore, exercises aimed at strengthening oral muscles can potentially improve mastication. Our findings of significant improvement in anterior and posterior tongue strength compared to baseline are consistent with previous studies demonstrating enhanced oral muscle strength after oral exercise [24,25,27]. Continued long-term use of smartphone-based oral strength training has the potential to improve oral health functions like mastication by strengthening oral muscles and promoting good occlusion.
However, a 2023 meta-analysis on the effects of oral strength training cautions against definitively attributing functional improvement solely to exercise [30]. While their analysis showed increased anterior and posterior tongue muscle strength in adults following oral exercises, it remains unclear if exercise alone leads to functional improvement. Similarly, a previous virtual reality study [13] reported non-significant but positive changes in oral strength after the program. These findings highlight the need for developing objective metrics and programs to definitively assess the effectiveness of training interventions.
The generalizability of the study findings requires caution due to the limited sample size recruited from specific regions. Additionally, while smartphone apps offer flexibility in scheduling, the training sessions were conducted at fixed times and locations to accommodate the participants, potentially hindering the full utilization of this advantage. Despite these limitations, the study demonstrates two key findings. First, the smartphone app-based oral muscle strengthening training program effectively improved oral health in older adults. Second, the program highlights the feasibility of smartphone app use for training purposes among this population. Moving forward, research should focus on developing strategies to integrate this smartphone app content seamlessly into older adults’ daily routines for practical application. Furthermore, investigating the long-term effects and sustainability of the training program is crucial for establishing its long-term value.
This study aimed to develop and evaluate the effectiveness of smartphone app-based educational content for oral musclestrengthening training in older adults. The training program consisted of 12 sessions delivered over six weeks, from late August to early October 2023. Sessions were conducted at participants’ affiliated facilities and lasted approximately 60 minutes each.
1. The program demonstrated significant effectiveness in promoting oral health. Compared to baseline measurements, participants experienced reductions in dental plaque (p<0.05), gingivitis (p<0.001), and tongue coating (p<0.01), along with increased salivation (p<0.001). Plaque decreased by 0.69 units, gingivitis by 0.99 units, tongue coating by 1.11 units, and salivation increased by 0.73 units. Post-hoc analysis revealed further significant differences between the experimental and control groups in terms of dental plaque (p<0.001), gingivitis (p<0.001), and tongue coating (p<0.05).
2. Oral muscle strength also improved significantly. ATS increased by 5.25 units (p<0.001), and PTS increased by 6.82 units (p<0.01).
The smartphone app content developed in this study holds promise for promoting oral health in older adults’ daily lives. Future efforts should focus on educating older adults about the app’s benefits and functionalities to encourage its use.
Conceptualization: KH Lee, YY Choi; Data collection: HY Moon, KJ Lee, MS Yoon; Formal analysis: ES Jung; Writing-original draft: KJ Lee; Writing-review and editing: YY Choi
The authors declared no conflicts of interest.
This project was conducted with the support of the National Research Foundation of Korea, funded by the government (Ministry of Science and ICT) (No. 2022R1A2C2010905).
This study was approved by the Institutional Review Board (IRB) of Shinhan University (IRB No. SHIRB-202307-HR-207-01).
None.
None.
1. Kang WS, Kim MS, Ko JU. Effects of the smartphone information use and performance on life satisfaction among older adults. J Korean Geron Soc 2013;33(1):199-214.
2. Shin YJ, Koo MJ. An explorative study on computer education for older adults and their life satisfaction. IJACE 2010;13(4):119-47. http://doi.org/10.22955/ace.13.4.201011.119
[DOI]
3. Kwak MJ, Roh SE, Kwak YG. The effect of informatization education satisfaction of elderly welfare center on elderly information usage and life satisfaction. J Korea Cont Assoc 2017;17(3):486-95. https://doi.org/10.5392/JKCA.2017.17.03.486
[DOI]
4. Shin JW, Kwon JS. An evaluative study on communication enhancement program through social network service of older adults in the community. J Korean Fam Soc Work 2017;58:151-79. https://doi.org/10.16975/kjfsw.2017.58.006
[DOI]
5. Kim YS. A study on relationships between health concern, health attitude and subjective health status, health practice of older adults [Master’s thesis]. Seoul: Seoul National University, 2002.
6. Lee HJ, Lee YS, Nam YO. Comparison of effectiveness on knowledge improvement before and after the oral health education: focusing on foreign students. J Korean Soc Dent Hyg 2016;16(1):85-92. https://doi.org/10.13065/jksdh.2016.16.01.85
[DOI]
7. Laguna L, Sarkar A, Artigas G, Chen J. A quantitative assessment of the eating capability in older adults individuals. Physiol Behav 2015;147:274-81. https://doi.org/10.1016/j.physbeh.2015.04.052
[DOI][PubMed]
8. Marshall TA, Warren JJ, Hand JS, Xie XJ, Stumbo PJ. Oral health, nutrient intake and dietary quality in the very old. J Am Dent 2002;133(10):1369-79. https://doi.org/10.14219/jada.archive.2002.0052
[DOI][PubMed]
9. Sagawa K, Furuya H, Ohara Y, Yoshida M, Hirano H, Iijima K, et al. Tongue function is important for masticatory performance in the healthy elderly: a cross-sectional survey of community-dwelling elderly. J Prosthodont Res 2019;63(1):31-4. https://doi.org/10.1016/j.jpor.2018.03.006
[DOI][PubMed]
10. Health Promotion Division of Health Center, KAMIKAMI oral exercise and oral care. Kochi city, Japan;2007: 1-8.
11. Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc 2005;53(9):1483-9. https://doi.org/10.1111/j.1532-5415.2005.53467.x
[DOI][PubMed]
12. Kim BH, Chung EJ. Oropharyngeal dysphagia in older adults. 2003;20(2):64-77. https://doi.org/10.1111/j.1741-2358.2003.00064.x.
[DOI][PubMed]
13. Choi YY. Jung ES, Lee KJ, Moon HY, Yoon MS, Lee KH. Effectiveness of virtual reality-based oral muscle strength training on oral function in aged. J Korean Soc Dent Hyg 2024;24(2):121-30. https://doi.org/10.13065/jksdh.20240013
[DOI]
14. Kang H. Sample size determination and power analysis using the G*power software. J Educ Eval Health Prof 2021;18:17. https://doi.org/10.3352/jeehp.2021.18.17
[DOI][PubMed][PMC]
15. Park JH, Kwon YC. Standardization of Korean version of mini-mental state examination (MMSE-K) for use in older adults. Part II. Diagnostic validity. J Korean Neuropsychiatr Assoc 1989;28(3):508-13.
16. Atchison KA, Dolan TA. Development of the geriatric oral health assessment index. J Dent Educ 1990;54(11):680-7. https://doi.org/10.1002/ j.0022-0337.1990.54.11.tb02481.x
[DOI][PubMed]
17. Locker D, Matear D, Stephens M, Lawrence H, Payne B. Comparison of the GOHAI and OHIP-14 as measures of the oral health-related quality of life of the elderly. Community Dent Oral Epidemiol 2008;29(5):373-81. https://doi.org/10.1111/j.1600-0528.2001.290507.x
[DOI][PubMed]
18. O’Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol 1972;43(1):38. https://doi.org/10.1902/jop.1972.43.1.38
[DOI][PubMed]
19. Winkel EG, Roldan S, Van Winkelhoff AJ, Herrera D, Sanz M. Clinical effects of a new mouthrinse containing chlorhexidine, cetylpyridinium chloride and zinc-lactate on oral halitosis. a dual-center, double-blind placebo-controlled study. J Clin Periodontol 2003;30(4):300-6. https://doi.org/10.1034/j.1600-051X.2003.00342.x
[DOI][PubMed]
20. Lὅe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand 1963;21(6):533-51. https://doi.org/10.3109/00016356309011240
[DOI][PubMed]
21. M Navazesh, C M Christensen. A comparison of whole mouth resting and stimulated salivary measurement procedures. J Dent Res 1982;61(10):1158-62. https://doi.org/10.1177/00220345820610100901
[DOI][PubMed]
22. Adams V, Mathisen B, Baines S, Lazarus C, Callister R. Reliability of measurements of tongue and hand strength and endurance using the Iowa oral performance instrument with healthy adults. Dysphagia 2014;29(1):83-95. https://doi.org/10.1007/s00455-013-9486-5
[DOI][PubMed]
23. Kim MY, Jun HJ. The effects of smartphone use on life satisfaction in older adults: the mediating role of participation in social activities. J Korean Geront Soc Wel 2017;72(3):343-70. https://doi.org/10.21194/kjgsw.72.3.201709.343
24. Jung ES, YY Choi, Lee KH. Effects of integrative cognitive function improvement program on cognitive function, oral health, and mental health in older people: a randomized clinical trial. Int J Environ Res Public Health 2022;19(21):14339. https://doi.org/10.3390/ ijerph192114339
[DOI][PubMed][PMC]
25. Jung ES, Lee KH, Seo SY. Effects of the integrated cognitive function improvement program on cognitive function and oral and mental health of middle-aged people: an application of non-face-to-face arbitration. J Korean Soc Dent Hyg 2023;23(1):43-53. https://doi.org/10.13065/jksdh.20230005
[DOI]
26. Lee KH, Jung ES, Choi YY. Effects of lingual exercises on oral muscle strength and salivary flow rate in elderly adults: a randomized clinical trial. Geriatr Gerontol Int 2020;20(7):697-703. https://doi.org/10.1111/ggi.13944
[DOI][PubMed]
27. Streckfus CF, Bigler LR. Saliva as a diagnostic fluid. Oral Dis 2002;8(2):69-76. https://doi.org/10.1034/j.1601-0825.2002.1o834.x
[DOI][PubMed]
28. Cho EP. Impact of oral function improving exercise on the oral function and quality of life in the elderly[Doctoral dissertation]. Daejeon: Chungnam National University, 2009.
29. Takahashi M, Koide K, Arakawa I, Mizuhashi F. Association between perioral muscle pressure and masticatory performance. J Oral Rehabil 2013;40(12):909-15. https://doi.org/10.1111/joor.12105
[DOI][PubMed]
30. Nathalya de FF, Andréa RM, Fernanda CF, Mariana RN, Elton M, Renata MMMF. The effects of lingual training: a systematic review with metaanalysis. Codas 2023;35(5):e20210324. https://doi.org/10.1590/2317-1782/20232021324pt
[DOI][PubMed]