1Department of Public Health Science, Graduate school of Natural Science, Dankook University
2Independent Researcher
3Department of Dental Hygiene, College of Health Science, Dankook University
Correspondence to Jong-Hwa Jang, Department of Dental Hygiene, College of Health Science, Dankook University, 119 Dandae-ro, Dongnam-gu, Cheonan-si, Chungcheongnam-do, Korea. Tel: +82-41-550-1495, E-mail: jhj@dankook.ac.kr
Volume 25, Number 2, Pages 89-99, April 2025.
J Korean Soc Dent Hyg 2025;25(2):89-99. https://doi.org/10.13065/jksdh.2025.25.2.1
Received on February 04, 2025, Revised on March 06, 2025, Accepted on March 12, 2025, Published on April 30, 2025.
Copyright © 2025 Journal of Korean Society of Dental Hygiene.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License(http://creativecommons.org/licenses/by-nc/4.0)
Objectives: Chewing discomfort (CD) is a predictor of poor oral and general health. Herein, we report a case in which we evaluated the effects of multi-oral muscle function improvement training (MoMFIT) for tongue pressure and masticatory function (bite force) conducted via home visits in an older adult. Methods: For 12 weeks, two trained dental hygienists visited the home of a denture-wearing older adult who complained of severe CD to conducted weekly MoMFIT sessions. MoMFIT comprises oral muscle massage, oral stretching exercises, tongue strength and pressure improvement training, and gum chewing exercises. Tongue pressure and bite force were measured at baseline (pre-intervention) and during the 9th and 12th MoMFIT sessions. Tongue pressure was determined as the maximum value after three measurements, and bite force was measured using a Prescale Film. Results: Tongue pressure increased by 58.6% in the 9th session (20.3 kPa) compared with the baseline (12.8 kPa) and by 72.7% in the 12th session (22.1 kPa). Compared with their pre-intervention values, the maximum and average bite forces increased by 58.9% and 12.7%, respectively, in the 12th session. Conclusions: Our data suggest that MoMFIT conducted via home visits can be a useful oral function rehabilitation program for denture-wearing older adults with CD.
Chewing discomfort, Community care, Denture, Older adults, Oral muscle function improvement
In response to the global trend of increasing life expectancy and the unprecedented pace of South Korea’s transition into a superaged society, a Pilot Project for Integrated Senior Care Support was developed and implemented at the governmental level [1]. The project laid the strategic groundwork for healthy ageing among community-dwelling older adults by linking home visit-based community integrated care services for older adults. Older adults who were eligible for participation in the pilot project from June 2019 to December 2023 were those in need of home-based care due to ageing, accidents, diseases, or disabilities and had systemic conditions, such as limited mobility, dementia, stroke, and depression [2].
Frailty refers to biological and physiological changes that result from ageing [3]. As older adults become more frail, they experience difficulties in adequately responding to weak external stimuli, which can result in hospitalisation, disability, or death [4]. The National Center for Geriatrics and Gerontology of Japan reported that oral frailty is a risk factor for general frailty [5]. That is, oral hypofunction may lead to general functional decline. According to the conceptual framework proposed by the Japanese Society of Gerodontology (JSG), oral hypofunction is diagnosed if the criteria for three or more signs or symptoms are met among the following seven signs or symptoms: poor oral hygiene, oral dryness, reduced occlusal force (bite force), decreased tongue-lip motor function, decreased tongue pressure, decreased masticatory function, and deterioration of swallowing function [6].
Mastication, an essential oral function, refers to the act of chewing with coordinated involvement of the teeth, tongue, cheeks, masticatory muscles, and maxilla and mandible (upper and lower jawbone), which work to grind the food into smaller pieces to form a bolus for easy swallowing [7]. As multiple organs are involved in the masticatory process, problems with any of them may limit food intake. Decreased masticatory performance is associated with tooth loss, reduced salivary flow, and reduced occlusal force [8]. In particular, the combined process of progressive muscle degeneration and loss of natural teeth among older adults can reduce mastication efficiency, resulting in difficulties in oral food intake compared with younger individuals [9]. The age-related loss of muscle bulk and functional decline in the intrinsic muscles of the tongue, geniohyoid muscle, and pharyngeal lumen are likely to cause problems in the 3-phase process of swallowing (oral, pharyngeal, and oesophageal phases) [10]. Muscles involved in swallowing can also influence bolus viscosity and volume and bolus transit time [11]. Moreover, malnutrition owing to swallowing dysfunction can lead to reduced muscle mass in the perioral muscles [12]. This can eventually cause choking and aspiration pneumonia.
Oral frailty is considered an early sign or symptom of physical frailty, causing a decline in oral health-related quality of life [13]. However, early detection of oral frailty can prevent frailty or facilitate recovery through relevant interventions [14]. Kim et al. [15] reported that a tongue strength training program combined with oral stretching exercises conducted among older adults aged 65 years and older improved their oral muscle functions. Previous case reports reported significant changes in the oral health status of older adults following the implementation of the home visit-based oral health care intervention program [16]. Although several previous studies have reported the effects of this intervention among older adults [1], there is a lack of research examining changes in oral muscle function following the intervention among older adults with chewing discomfort (CD) wearing dentures. Therefore, in this study, we evaluated the effects of the MoMFIT intervention administered via home visits as the Pilot Project for Integrated Senior Care Support (ISCS) on tongue pressure and masticatory function to provide valuable insights into improving oral healthrelated quality of life among denture-wearing older adults with CD.
This case report evaluated changes in tongue pressure and masticatory function of an older adult following the MoMFIT intervention through home visits among participants in the ISCS conducted in Cheonan-si, Chungcheongnam-do, South Korea. Participants in the ISCS-based MoMFIT intervention underwent an oral health assessment conducted by a dentist.
The training process of the MoMFIT intervention consisted of 1) oral muscle stretching, 2) tongue strengthening training, and 3) chewing exercises [16]. First, oral muscle stretching flexibly strengthens the muscles around the oral cavity through oral muscle massage (1 min) and oral oral exercises (4 min) training. Second, tongue strengthening training improves swallowing function by raising the tongue to the palate to make a ticking sound (2 min), followed by tongue strengthening training using a Peco-Panda (3 min). Last, the chewing exercise (5 min) is a process of chewing gum once a day, forming the gum into a ball using the tongue, placing it in the middle of the tongue, pausing for a moment, and then spitting it out on a tissue to strengthen the mastication and swallowing functions.
The inclusion criteria for the participant in this case report were 1) an older adult aged 65 years or older with CD, 2) an older adult wearing dentures or with CD due to wearing new dentures, and 3) an older adult with the Korean version of Mini-Mental State Examination (K-MMSE) scores of 24 or higher to enable oral muscle function improvement training. The exclusion criteria were 1) an individual under 65 years of age who does not wear dentures and 2) one with K-MMSE scores of less than 24 points.
This study followed the Declaration of Helsinki and the CARE checklist for case reports [17]. Regarding ethical considerations, the study protocol was approved by the Institutional Review Board of Dankook University (DKU 2023-10-039 on 20 December 2023). Upon obtaining consent from the participant, photos, including intraoral photographs, were taken, and the tongue pressure and bite force were measured <Fig. 1>.

Fig. 1.Intraoral status of the patient
The participant was a 78-year-old woman with a history of limited mobility, hearing impairment, hypertension, arthritis, heart disease, gastrointestinal disorders, and headaches. According to the oral examination by a dentist before starting the MoMFIT intervention, the maxilla was wearing a partial denture, and the mandible was edentulous and wearing a complete denture. The patient’s K-MMSE, which evaluates cognitive function, was 26 points. She was a denture wearer but participated in the MoMFIT interventions with little or no use of dentures. In week 7 of the intervention, she complained of severe oral discomfort due to maladaptation to wearing new dentures, but this gradually improved. She complained of discomfort related to wearing dentures due to dry mouth and pain in the mandibular gums when chewing, and she was not using denture adhesive. The dentures were removed during the MoMFIT intervention when she complained of severe oral discomfort. However, for sessions with mild oral discomfort, the dentures were kept in place as much as possible during the intervention.
From March 1 to May 24, 2024, two dental hygienists visited the participant’s home and administered weekly MoMFIT interventions for 12 sessions. The MoMFIT intervention program comprised oral muscle stretching (oral muscle massage and oral stretching exercises), tongue strength improvement training (clock sound training and tongue pressure training), and chewing exercises with chewing gum.
Oral function assessment was performed at baseline, week 9 of the MoMFIT intervention, and week 12 of the MoMFIT intervention in order to observe changes in the oral function <Fig. 2>. The oral function was assessed by measuring tongue pressure and bite force. Tongue pressure was measured using the JMS tongue pressure meter (Japan Medical Supply Co., Ltd., Japan), and this method enabled safe and convenient testing with quantitative measurements of the outcomes. The maximum tongue pressure generated between the tongue and the palate was defined as the maximum value from measuring the force of the tongue pressing the tongue pressure probe against the palate three times. Dental Prescale II (GC Co., Tokyo, Japan), a pressure-indicating sensor film, was used to assess the bite force. According to the guidelines of the JSG, a patient is diagnosed with decreased bite force when the bite force is less than 500 N on the Dental Prescale II.
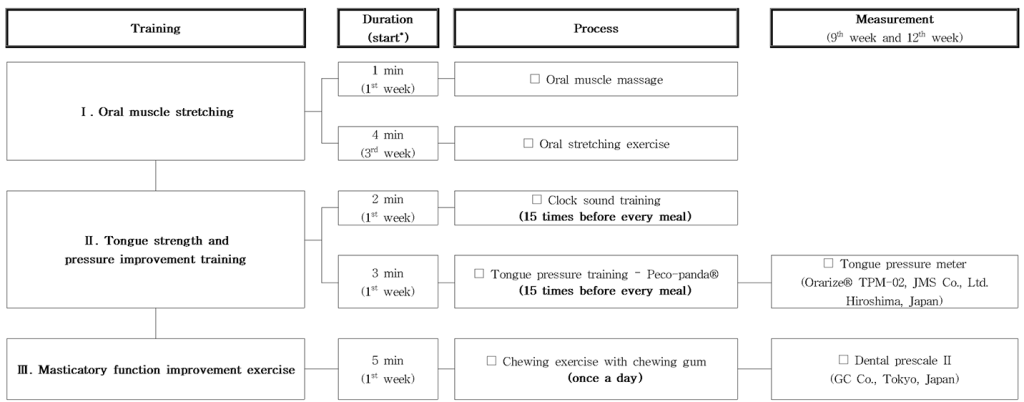
Fig. 2. Process of the multi-oral muscle function improvement training (MoMFIT) intervention through home visits for oral muscle function improvement. *Training was performed from the starting week to the 12th week
The oral muscle massage developed by Park et al. [16], performed by the ‘intervention team’ in this study, is a method of simultaneously massaging the muscles inside and outside the mouth using the thumb and index finger at six points: the middle point of the upper and lower masticatory muscles, the intersection of the masticatory and lip muscles, and the exact centre of the lip muscles.
The ‘intervention team’ provided the study participant with a video on oral muscle massage [18] (from the Korea Association for Oral Health) and conducted hands-on training with the guardians (caregivers) and care workers to enable the participant to perform the massage independently <Fig. 3>.
The oral stretching exercise comprised nine different exercises, including preparatory exercise, oral exercises for saliva flow, speaking, swallowing, and chewing. In line with previous studies, the ‘intervention team’ focused on improving dysphagia by starting with preparatory exercises and then concentrating on oral exercises to promote salivary flow to alleviate oral dryness. As the participant became accustomed to wearing the new denture, oral exercises to improve speaking with accurate [pa], [ta], [ka], and [ra] pronunciation were performed. In particular, oral exercises to improve swallowing were performed for participants with difficulties due to frequent choking by strengthening the muscles surrounding the bronchi and oesophagus. Each exercise was performed for 8 seconds. All home visit-based participants involved in the oral health care intervention program received the oral stretching exercise calendar for use at home.

Fig. 3. Oral muscle stretching. For more information, please refer to the following link
(https://youtu.be/9vcu5sNuEuk?si=99So_cQF2Wb2_8OW by the Korea Association for Oral Health)
The clock sound training is a tongue strength improvement training in which the tongue touches the palate with the lips closed so that the upper and lower teeth are not clenched tightly, and the lower jaw is raised upwards to help the lips close [19]. It is designed to improve the muscle strength of the tongue, making “tick, tock” sounds similar to clock sounds <Fig. 4>. The patient was instructed to undergo clock sound training thrice daily before meals, with 15 movements in each session.
To strengthen the tongue muscles necessary for swallowing, a non-medical device called ‘Peco-Panda’ (a tongue training device) was used, which allows easy training for anyone. The participants were instructed to use the device thrice daily with 15 repetitions per set. According to Tanaka et al. [20], based on the reference value for the maximum tongue pressure for adults aged 70 years or older, a tongue pressure ≥30 kPa was set as the target. First, the patient was given Pink Panda (10 kPa), the lowest pressure level, to start tongue strength training. This pressure was replaced with the Purple Panda (15 kPa) and Green Panda (20 kPa) to gradually increase tongue pressure. In the 12 home visits, from the second visit, the participant was encouraged to perform the training by herself after explaining the purpose of the tongue strength improvement training. For each visit, the motions of the participant’s training were recorded on videos to provide monitoring and feedback.
Our patient’s tongue pressure before the MoMFIT intervention was 12.8 kPa. This pressure increased to 20.3 kPa by week 9 (approximately a 58% increase) and then to 22.1 kPa by week 12 (approximately a 72% increase) <Fig. 4>. These improvements indicated that despite a decrease in the amount and frequency of food intake due to pain caused by the new denture, healthy tongue strength was maintained through continuous and incremental home visit-based oral health care interventions.

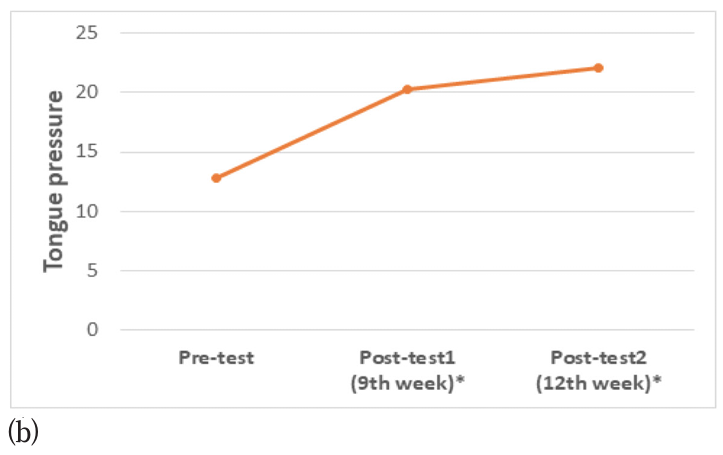
Fig. 4. Tongue strength and pressure improvement training: (a) clock sound training and (b) changes in tongue pressure.
Considering the patient’s age, chewing exercises were performed using xylitol green chewing gum, which is less sticky and does not easily adhere to dentures. Xylitol green chewing gum was provided once a day for daily chewing exercises, and the participant was instructed not to chew for more than 20 minutes to reduce jaw strain. To increase her tongue strength, the gum was chewed into a spherical shape in her mouth, placed in the middle of the tongue, held briefly, and then spat out to observe its shape. If the gum adhered to the denture, the denture was removed, and training was resumed. For the participant who had visited the dentist for a new denture, chewing exercises were initially performed with the new denture so that the participant could adapt to the new denture. If she complained of any discomfort, training was conducted without the denture. After 12 sessions of the intervention program, owing to the effect of the chewing exercise, the participant was able to shape the gum into a completely spherical shape compared with the shape at the start of the intervention. At the start of gum-chewing training, the shape of the gum formed using the tongue was irregular. However, it became somewhat spherical by week 6, and it was completely spherical at week 10. This showed improved bite force and tongue movement <Fig. 5>.
The bite force evaluation using the Prescale Film revealed that the average bite pressure increased from 24.0 MPa at week 9 to 27.6 MPa at week 12. Moreover, the maximum bite force increased from 51.1 N at week 9 to 99.9 N at week 12 <Fig. 5>. A notable feature of the participant’s oral condition was that by week 9, left occlusion was not experienced due to the new denture; however, continuous and incremental oral muscle function training markedly improved the bite force by week 12.
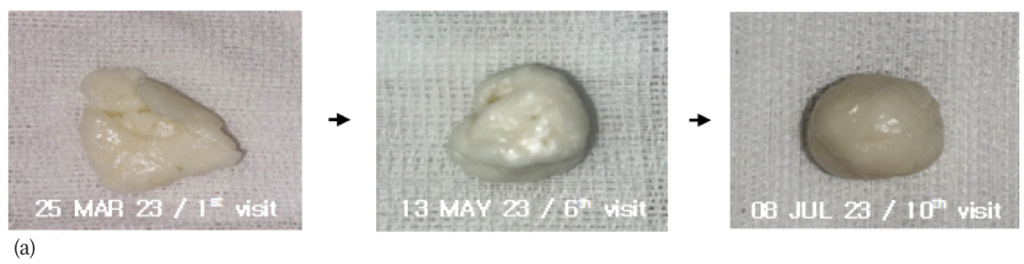
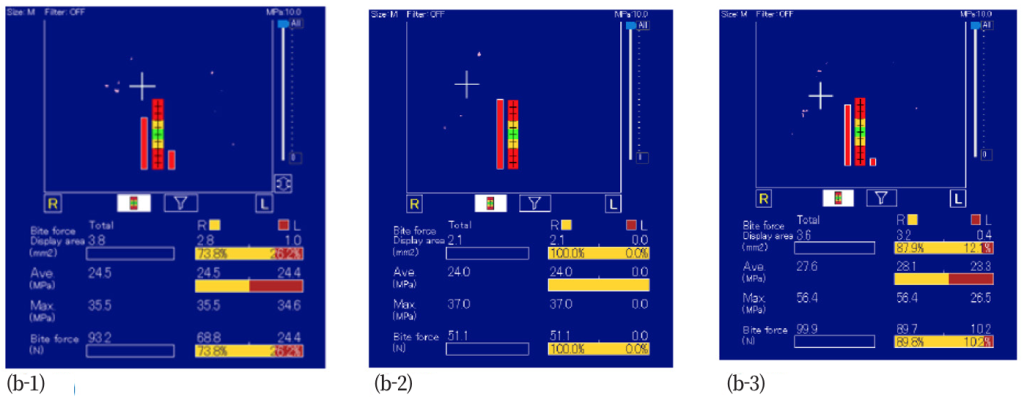
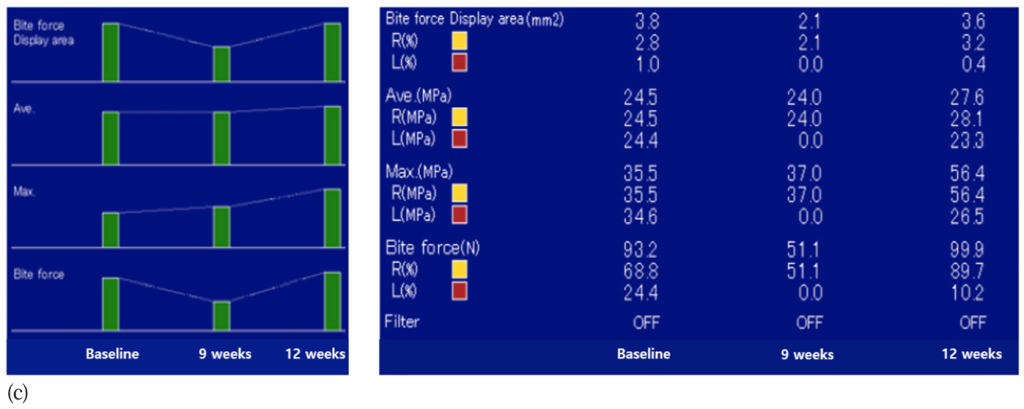
Fig. 5. Masticatory function improvement exercise; (a) change in gum shape after chewing gum training; (b-1) bite force at baseline; (b-2) bite force at 9th week; (b-3) bite force at 12th week; (c) Changes in bite force at baseline, 9th weeks, and 12th weeks.
Oral health is closely associated with general health. With ageing, older adults may develop sarcopenic dysphagia (swallowing disorder owing to loss of muscle mass), resulting in a decline in their quality of life [15]. Therefore, this study examined a patient who achieved improved bite force and tongue strength after receiving the MoMFIT intervention under a home visit-based oral health care program based on the Pilot Project for ISCS.
The patient was taking medication for hypertension, arthritis, heart disease, gastrointestinal disorders, and headache and complained of severe discomfort due to dry mouth, requiring treatment. In this study, the patient reported a reduction in CD and an improvement in chewing ability after the MoMFIT intervention.
Min and Lee [19] investigated effective interventions for paediatric feeding disorders with neuromuscular diseases. They reported that, as oral motor skills decrease with disease progression, interventions with oral exercises are needed to reduce fatigue in the neck, oral, and facial muscles. Umay et al. [21] reported that age-associated sarcopenia was associated with dysphagia. Notably, among the muscles involved in swallowing, the risk of developing dysphagia increases with decreasing masseter muscle thickness. In the speciality of services provided in dental hospitals and clinics, specialised departments such as the Preventive Dentistry Clinic, the Dental Clinic for People with Disabilities, and the Paediatric Dentistry Clinic are available according to the needs of patients. However, geriatric dentistry (a speciality in dental care for older adults) has not been established as a specialised service [22].
Park et al. [16] reported improved oral muscle function and positive changes in subjective oral health status after providing professional oral hygiene care and tongue pressure improvement training for older adults with visual or hearing impairments through a home-based oral health care intervention. Raj et al. [23] reported that among older adults living in a nursing home, oral exercises targeting facial muscles, the tongue, salivary glands, and swallowing increased the amount of salivary secretion and decreased salivary pH and xerostomia.
A self-resistance exercise in which the tongue is pushed against the palate helps develop the ability to easily generate tonguepalate pressure without the need for special equipment or restrictions [24]. Clock sound training does not require a separate tool, so that an older adult can perform the training anytime and anywhere.
The maximum tongue pressure of older adults aged 70 years or older is significantly lower than that of adults in their 20s–50s [20]. Moreover, the diet of older adults should be adjusted based on their tongue pressure levels [20]. This is because normal diet intake is possible when the tongue pressure is ≥25 kPa. However, adjusted food intake is more likely when the tongue pressure is <20 kPa [20].
In our case, the patient underwent clock sound training, a method that can be conducted easily regardless of the patient’s location, and tongue pressure improvement training using Peco-Panda. As a result, positive changes were observed, including increased tongue pressure. This result was consistent with Chiba [25] findings, in which older adults underwent training involving the pronunciation of [Pa], [Ta], and [Ka] sounds in a loud voice, which stimulated muscle movements of the tongue (front, middle, and base), leading to improvements in pronunciation and tongue movements. Using Peco-Panda, improvements were noted in tongue strength for swallowing, tongue endurance to consume adequate amounts of food, and tongue coordination to efficiently gather and swallow chewed food.
In addition, in our patient, when the chewing exercise was performed with xylitol green chewing gum, the spherical shape of the gum produced through continuous and incremental oral muscle function training demonstrated that the training had a positive effect on stabilising the location of the tongue and improving tongue strength, despite the participant changing from old to new dentures after tooth extraction. This finding is consistent with that of Kashiwazaki et al. [26], in which older adults underwent gum chewing exercises for 2 months and achieved improved bite force and tongue strength due to stimulation of masticatory and tongue motor functions. Chewing gum training among older adults [27] has been shown to improve oral function and mastication, which are closely related to bite force. Bite force refers to the force exerted on the teeth and supporting structures when chewing food, as the movement of the masticatory muscles affects bite force [28]. Following the measurement of the participant’s bite force using the Dental Prescale II, the bite force decreased at week 9 (51.1 N) compared with the pre-intervention level (93.2 N) because the patient started wearing new dentures at week 9 of the intervention and was not familiar with the denture. However, compared with the values at week 9, at week 12, the bite force (99.9 N) increased by approximately 95%, the maximum bite pressure (56.4 MPa) increased by 52%, and the average bite pressure (27.6 MPa) increased by 15%. Compared with the finding of previous study, which reported average bite pressure (31.1±8.8 MPa) and maximum bite force (173.6±168.5 N) for patients wearing general removable partial dentures, our results were somewhat lower [29]. Nevertheless, following the 12 sessions of intervention, our patient showed improved average bite pressure and maximum bite force. These findings indicate that rehabilitation involving oral exercise should be conducted to prevent a decline in masticatory performance in older adults.
A decline in the oral health-related quality of life of older adults leads to a decrease in the general health-related quality of life. Therefore, identifying the causes of oral hypofunction and systematic interventions to prevent oral hypofunction is necessary by implementing adequate oral muscle function improvement training [15]. Ongoing oral care tailored to individual older adults and oral health education should be implemented to help improve oral muscle function, swallowing function, and oral hygiene management [16].
This study provided oral muscle function improvement training through home visits for a denture-wearing older adult with hearing impairment and severe CD. The results confirmed the intervention’s ability to improve oral muscle functions, including masticatory function (bite force) and tongue strength. This study demonstrates the clinical significance of a preventive oral-motor function rehabilitation program for community-dwelling older adults with CD, particularly those who are edentulous and wear dentures. The positive outcomes achieved in this study can serve as a representative case to lay the foundation for the expanded application of home visit-based oral health intervention activities in community-based oral health services in this era of an ageing society or a super-aged society. The MoMFIT intervention was applied to an older adult wearing dentures, but it can be applied to all individuals who require strengthening of the oral muscles. In particular, oral health improvements are expected to be more pronounced among patients who visit clinics to treat discomfort due to dry mouth and age-related oral muscle dysfunction.
However, since the effects of oral health interventions may depend on multiple factors, including differences in the general and health-related characteristics of older adults, it is difficult to quantitatively assess the efficacy of the intervention based on the outcomes of a single participant reported in this case report. In addition, for the MoMFIT intervention to become generalised, institutional support is needed to secure professional manpower and financial resources to enable community-centred MoMFIT programs. Therefore, future research should use randomised controlled clinical trials to evaluate the effectiveness of interventions with high-quality evidence.
In addition, continuous oral healthcare, not one-off service, is necessary to maintain and improve the oral health of older adults and enhance their oral health-related quality of life. After the home-visit-based oral health management program concludes, education should be provided to ensure that individual older adults can perform self-oral hygiene management and continue their oral muscle function training. Furthermore, digital applications with educational content can be developed for the MoMFIT program and widely adopted by non-experts in long-term care facilities to improve the oral health of community-dwelling older adults via integrated care.
A MoMFIT program comprising oral muscle stretching, tongue strength improvement training, and masticatory function training was administered by experts once a week for 12 weeks to a community-dwelling older adult who complained of CD.
1. The MoMFIT program improved effectively tongue strength and masticatory function (bite force) of a denture-wearing older adult.
2. Oral muscle function improvement training tailored to individual older adults through home visits was effective in maintaining and improving the oral muscle strength of our patient.
3. Tailored home-visit training can improve the masticatory performance of patients with CD or those wearing new dentures.
Therefore, we propose that the MoMFIT, delivered through home visits, will serve as a useful oral function rehabilitation program for denture-wearing older adults with CD.
Conceptualization: JH Jang, MH Park, MS Jeong; Data collection: MH Park, JW Park, HS Oh, MS Jeong; Formal analysis: MH Park; Writing-original draft: MH Park, JH Jang; Writing-review&editing: MH Park, JW Park, HS Oh, MS Jeong, JH Jang
JH Jang has been a member of editorial committee of the Journal of Korean Society of Dental Hygiene. She is not involved in the review process of this manuscript. Otherwise, there was no conflicts of interest.
This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2023S1A5A2A01077353).
This study was approved by the Institutional Review Board (IRB) of Dankook University (IRB No. DKU 2023-10-039 on 20 December 2023).
Data can be obtained from the corresponding author.
None.
1. Jang JH. Oral health care intervention protocol for older adults at home in dental hygienists: a narrative literature review. J Korean Soc Dent Hyg 2023;23(5):333-41. https://doi.org/10.13065/jksdh.20230037
[DOI]
2. Lee SG, Ko SM, So JS, Kwak JM, Park II, Lee JN, et al. Proposal for introducing community oral care/palliative treatment system. J Korean Acad Geriatr Dent 2022;18(1):19-28.
3. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56(3):M146-M57. https://doi.org/10.1093/gerona/56.3.m146
[DOI][PubMed]
4. Hwang HS, Kwon IS, Park BJ, Cho BL, Yoon JL, Won CW. The validity and reliability of Korean frailty index. J Korean Geriatr Soc 2010;14(4):191202. https://doi.org/10.4235/jkgs.2010.14.4.191
[DOI]
5. Jung HI. Frailty in older people and oral frailty. J Korean Dent Assoc 2020;58(12):746-50. https://doi.org/10.22974/jkda.2020.58.12.003
[DOI]
6. Minakuchi S, Tsuga K, Ikebe K, Ueda T, Tamura F, Nagao K, et al. Oral hypofunction in the older population: position paper of the Japanese society of gerodontology in 2016. Gerodontology 2018;35(4):317-24. https://doi.org/10.1111/ger.12347
[DOI][PubMed]
7. Okeson JP. Management of temporomandibular disorders and occlusion. 6th ed. Elsevier Health Sciences: Amsterdam: Netherlands; 2007: 1-36.
8. Ikebe K, Matsuda K, Morii K, Furuya-Yoshinaka M, Nokubi T, Renner RP. Association of masticatory performance with age, posterior occlusal contacts, occlusal force, and salivary flow in older adults. Int J Prosthodont 2006;19(5):475-81.
9. Laguna L, Sarkar A, Artigas G, Chen J. A quantitative assessment of the eating capability in the elderly individuals. Physiol Behav 2015;147:274-81. https://doi.org/10.1016/j.physbeh.2015.04.052
[DOI][PubMed]
10. Molfenter SM, Amin MR, Branski RC, Brumm JD, Hagiwara M, Roof SA, et al. Age-related changes in pharyngeal lumen size: a retrospective MRI analysis. Dysphagia 2015;30(3):321-7. https://doi.org/10.1007/s00455-015-9602-9
[DOI][PubMed]
11. Park MJ, Woo HS, Chang KY, Han MY. Comparison of sEMG activation on swallowing-related muscles according to the bolus viscosity and volume. J Korean Soc Occup Ther 2012;20(4):69-80.
12. Dellis S, Papadopoulou S, Krikonis K, Zigras F. Sarcopenic dysphagia: a narrative review. J Frailty Sarcopenia Falls 2018;3(1):1-7. https://doi.org/10.22540/JFSF-03-001
[DOI][PubMed][PMC]
13. Lim HD. The important consideration for healthy life of older age; frailty and oral frailty. J Korean Dent Assoc 2022;61(1):59-66. https://doi.org/10.22974/jkda.2022.61.1.004
[DOI]
14. Dent E, Morley JE, Cruz-Jentoft AJ, Woodhouse L, Rodríguez-mañas L, Fried LP, et al. Physical frailty: ICFSR international clinical practice guidelines for identification and management. J Nutr Health Aging 2019;23(9):771-87. https://doi.org/10.1007/s12603-019-1273-z
[DOI][PubMed][PMC]
15. Kim NS, Lee JH. Effects of tongue strength training program combined with oral exercises on swallowing disorder, swallowing ability, and tongue pressure in the elderly. J Korean Soc Dent Hyg 2023;23(2):105-13. https://doi.org/10.13065/jksdh.20230011
[DOI]
16. Park MH, Jeong MS, Jang JH. Changes in concentration of VSCs after home oral care interventions based on community care in older adults. J Korean Soc Dent Hyg 2023;23(2):91-103. https://doi.org/10.13065/jksdh.20230010
[DOI]
17. Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache 2013;53(10):1541-7. https://doi.org/10.1111/head.12246
[DOI][PubMed]
18. Korea Association for Oral Health. Community care-based oral health education materials for the elderly [Internet]. Korea Association for Oral Health; 2020[cited 2024 Aug 09]. Available from: https://www.dental.or.kr/dental_data3.php.
19. Min KC, Lee JS. Characteristics and interventions in paediatric feeding disorder with neuromuscular diseases. J Korean Acad Dysphagia Rehabil 2020;3(2):1-11. https://doi.org/10.31115/sr.2020.3.2.1
[DOI]
20. Tanaka Y, Nakano Y, Yokoo M, Takeda Y, Yamada K, Kayashita J. Examination about the relation of meal form, tongue pressure, grip and walking state in inpatient and elderly residents. Japanese J Dysphagia Rehabil 2015;19(1):52-62. https://doi.org/10.32136/jsdr.19.1_52
[DOI]
21. Umay E, Akaltun MS, Uz C. Association between swallowing muscle mass and dysphagia in older adults: a case-control study. J Oral Rehabil 2023;50(6):429-39. https://doi.org/10.1111/joor.13439
[DOI][PubMed]
22. Kang KL, Kang MS, So JS, Ko SM, Han SR, Hwang JY, et al. The teaching of geriatric dentistry in South Korean dental schools. Gerodontology 2022;40(2):238-43. https://doi.org/10.1111/ger.12647
[DOI][PubMed]
23. Raj BT, Sreelekha B, Manjula A. Effectiveness of oral exercise on oral function among the elderly. J Family Med Prim Care 2020;9(4):1896-903. https://doi.org/10.4103/jfmpc.jfmpc_899_19
[DOI][PubMed][PMC]
24. Nam KW. Effects of a tongue self-resistance exercise on the swallowing function of patients with stroke: case report. Ther Sci Rehabil 2018;7(4):43-55. https://doi.org/10.22683/tsnr.2018.7.4.043
[DOI]
25. Chiba Y. Short-term effectiveness of a swallowing exercise for the elderly using day-care services. J Nurs Care 2013;S5:1-7. https://doi.org/10.4172/2167-1168.S5-012
[DOI]
26. Kashiwazaki K, Komagamine Y, Shanglin W, Ren X, Hayashi N, Nakayama M, et al. Improvements in maximum bite force with gum-chewing training in older adults: a randomized controlled trial. J Clin Med 2023;12(20):6534. https://doi.org/10.3390/jcm12206534
[DOI][PubMed][PMC]
27. Taguchi C, Takeuchi R, Yano G, Suzuki H, Sakadume H, Nagashima T, et al. Intervention effect of chewing gum mastication in residents and users of elderly facility. Int J Oral Med Sci 2023;21(3):100-11. https://doi.org/10.5466/ijoms.21.100
[DOI]
28. Koc D, Dogan A, Bek B. Bite force and influential factors on bite force measurements: a literature review. Eur J Dent 2010;4(2):223-32. https://doi.org/10.1055/s-0039-1697833
[DOI][PubMed][PMC]
29. Choi SH, Choi YS, Lee JH, Ha SR. Evaluation of occlusal strength using T-Scan Novus and Dental prescale II in dental prosthodontic treatments: a case report. J Korean Acad Prosthodont 2023;61(2):160-78. https://doi.org/10.4047/jkap.2023.61.2.160
[DOI]