1Department of Dental Hygiene, Taegu Science University
2Department of Dental Hygiene, Choonhae College of Health Science
3Department of Dental Hygiene, Dong-eui University
Correspondence to Jung-Hwa Lee, Department of Dental Hygiene, College of Nursing and Healthcare Sciences, Dong-eui University, 176 Eomgwang-ro, Busanjin-gu, Busan-si, 47340, Korea. Tel: +82-51-890-4239, Fax: +82-505-182-6878, E-mail: yamako93@naver.com
Volume 25, Number 4, Pages 285-96, August 2025.
J Korean Soc Dent Hyg 2025;25(4):285-96. https://doi.org/10.13065/jksdh.2025.25.4.2
Received on April 30, 2025, Revised on July 15, 2025, Accepted on July 31, 2025, Published on August 30, 2025.
Copyright © 2025 Journal of Korean Society of Dental Hygiene.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License(http://creativecommons.org/licenses/by-nc/4.0).
Objectives: The aim of this was to evaluate the effects of an oral myofunctional exercise program on improving oral function in older adults who use welfare tubes. Methods: We recruited 37 older adults who had used the Gyeongbuk Community Welfare Center for approximately four months between June and October 2022. The control group completed a questionnaire and an objective oral myofunction assessment, whereas the experimental group participated in an oral myofunction exercise program. The program was conducted twice weekly for 8 weeks at a community center. Objective oral health assessments were performed in both groups before, during, and after, 4 and 8 weeks after the start of the intervention period. Results: As a result of the oral myofunctional exercise program, a comparison of the subjects bite force (p=0.008), tongue pressure (p=0.003), maximum mouth opening (p<0.001), and alternating Diadochokinesis (DDK) (p<0.001) showed that the experimental group had greater improvements than the control group. Conclusions: Based on these findings, oral myofunctional exercise-such as chewing silicone straws and playing harmonica-should be incorporated into the existing oral health programs in public health centers and welfare facilities for older adults.
Masticatory function, Myofunctional therapy, Older adults, Oral function
The proportion of South Korea’s population aged 65 years and older is projected to rise markedly, from 17.4% in 2022 to 20% by 2025, 30% by 2036, and ultimately 40% by 2050 [1]. This demographic transition has intensified concerns about the quality of life and health issues confronting the elderly population [2]. The proportion of South Korea’s population aged 65 years and older is projected to rise markedly, from 17.4% in 2022 to 20% by 2025, 30% by 2036, and ultimately 40% by 2050 [1]. This demographic transition has intensified concerns about the quality of life and health issues confronting the elderly population [2]. Age-related sarcopenia is a common condition among elderly individuals, characterized by a decline in muscle mass accompanied by reductions in muscle strength and functional performance. This gradual degeneration contributes to the onset of osteoporosis, heightened susceptibility to falls, diabetes, dementia, cardiovascular disorders, and a range of additional health issues, ultimately leading to decreased quality of life and increased mortality [3].
The gradual decline in muscle function observed with aging leads to a reduction in the strength of the perioral musculature, which includes the masticatory muscles critical for chewing, as well as the tongue and orbicularis oris muscles that play key roles in swallowing. This deterioration adversely affects mastication, deglutition, and speech articulation in elderly individuals, thereby compromising overall oral muscle performance [4,5]. The masticatory muscles, including the masseter, temporalis, medial pterygoid, and lateral pterygoid, are essential for enabling chewing movements [6]. A reduction in the strength of these muscles can lead to impaired mastication and difficulties in food intake among elderly individuals, potentially resulting in digestive issues and nutritional deficiencies. Such conditions negatively affect overall health and quality of life. Therefore, maintaining adequate muscle strength and mass in the masticatory muscles is crucial for preserving normal masticatory function [7].
The strength of the tongue musculature plays a crucial role in maintaining essential oral functions, such as the regulation of tooth alignment, speech articulation, and the swallowing mechanism [8]. A decline in tongue muscle strength has been correlated with dysphagia, a disorder characterized by impaired speech production, difficulties in forming food boluses during swallowing, premature leakage of oral food residues into the pharynx, and subsequent aspiration of these residues into the epiglottis [9]. The importance of tongue strength is further highlighted by epidemiological data indicating that 33.7% of elderly individuals in Korea experience dysphagia, a condition associated with a sevenfold increase in the risk of aspiration pneumonia, which may be fatal in severe cases [10]. The orbicularis oculi muscle is integral not only to facial expression but also to essential functions including mastication, articulation, and swallowing [11]. In elderly individuals, diminished strength of this muscle can result in challenges during communal eating, as it may permit the escape of food from the oral cavity. Such functional impairments have the potential to adversely impact self-esteem and may lead to social withdrawal [4]. Moreover, challenges in producing bilabial sounds can result in communication difficulties, which may adversely impact interpersonal relationships and social participation. Such impediments can obstruct social interactions and potentially contribute to social isolation [12].
The significance of oral motor function has led to a growing body of research examining the effects of aging on oral motor abilities. These studies encompass the maintenance of oral motor skills and masticatory function and their influence on the quality of life among older adults [13], the association between cognitive function and chewing capacity in elderly individuals [14], as well as the improvement of oral function through targeted oral exercise interventions [15].
The oral cavity comprises small, complex muscles that necessitate precise motor control. Consequently, an interactive methodology grounded in direct assessment and participant feedback is imperative [16]. However, the majority of previous studies have concentrated on isolated muscle-strengthening exercises aimed at specific anatomical components, such as the tongue and lips. This methodology presents limitations in enhancing comprehensive oral muscle function. Consequently, it is imperative to design more holistic and systematic intervention programs, accompanied by thorough validation of their effectiveness [6,17].
This study incorporated three exercises that have been previously validated for their effectiveness in the literature. Kim et al. [18] established that simple oral exercises (SOE) and gum chewing significantly improve masticatory function. However, due to the limitations encountered by denture wearers, the current research employed straw biting and chewing as substitutes for gum chewing to enhance the strength of the lip and tongue muscles. Furthermore, harmonica playing functions as an effective method for strengthening the oral musculature involved in articulation and for enhancing respiratory function through the repetitive engagement of the lips, tongue, and jaw muscles [19]. In addition, exercises that involve alternation of articulatory movements have been shown to improve the regulation of oral muscles and to augment speech intelligibility by activating various articulatory components [13].
Accordingly, the current study aimed to design and implement a regimen of oral muscle function exercises—including activities such as straw biting, harmonica blowing, and articulation alternation—with the purpose of improving oral muscle function in elderly participants and evaluating the effectiveness of the intervention.
The study population comprised elderly individuals aged 65 years and above who accessed the senior welfare center located in Y city, Gyeongsangbuk-do. Participants voluntarily consented to partake in the research following a detailed explanation of the study’s objectives and procedures provided through the researcher’s recruitment announcement.
The inclusion criteria for this study encompassed individuals without previous experience in managing temporomandibular joint disorder, those not diagnosed with xerostomia or Sjögren’s syndrome, participants without edentulism or complete dentures, individuals possessing adequate masticatory and speech functions, and those capable of complying with oral muscle function evaluations and completing related questionnaires.
The calculated sample size required for the study was 34 participants, based on a significance level of 0.05, a statistical power of 0.80, and an effect size of 0.50 for repeated measures analysis of variance, as determined using the G*power 3.1 software. Accounting for an anticipated dropout rate of 20%, the target sample size was adjusted to 41 participants. Ultimately, the final analysis comprised data from 37 participants who completed the oral muscle function exercise program, which was conducted over approximately four months, from June 2022 to October 2022, excluding those who withdrew during the intervention period.
Participants were randomly allocated to one of two groups: an experimental group (n=20) that participated in a regimen of oral muscle function exercises, and a control group (n=17) that did not undergo any intervention. The study protocol was reviewed and approved by the Institutional Review Board of Dong-eui University to ensure ethical and scientific rigor (IRB: DIRB-202205-HR-E-10).
To assess the impact of the oral muscle function exercise program on enhancing oral muscle function, a single-blind study design was implemented, wherein participants were randomly allocated to either the experimental or control group. Participants remained unaware of their group assignment to mitigate expectancy effects and thereby increase the objectivity of the investigation.
The experimental group engaged in an oral muscle function exercise regimen, which comprised activities such as straw biting and chewing, harmonica blowing, and articulatory alternation exercises, conducted twice weekly over an eight-week period, amounting to a total of 16 sessions. In contrast, the control group did not undergo this intervention.
To evaluate alterations in oral muscle function, assessments of bite force, tongue strength, maximal mouth opening, and articulatory alternation movements were conducted prior to the intervention, as well as at 4 and 8 weeks following its completion in both groups. The study timeline is depicted in <Fig. 1>.
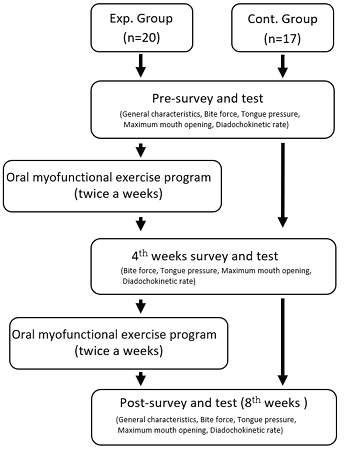
Fig. 1. Design of this study
The participants attended the senior welfare center biweekly, from 10:00 a.m. to 12:00 p.m., over a period of eight weeks, during which they engaged in an oral muscle function exercise program facilitated by the researcher.
General characteristics, including gender, age, smoking status, presence of systemic diseases, and medication usage, alongside oral health-related factors such as denture use, frequency of daily tooth brushing, and tongue cleaning practices, were evaluated through a set of eight structured questions.
(1) Straw biting and chewing
This study utilized the oral motor facilitation technique (OMFT) as developed by Min et al. [19]. Given that the participants were elderly individuals aged 65 years and above, they were instructed to perform chewing exercises consisting of 100 repetitions twice daily—once prior to breakfast and once prior to dinner—using a baby silicone straw measuring 23.5 cm in length and 1 cm in outer diameter.
(2) Playing the harmonica
In reference to the investigation conducted by Lee and Kang [20] on oral motor activities involving harmonica performance, the present study required participants to play the piece ‘Little Star’ employing the vibrato technique for a duration of 10 minutes daily.
(3) Articulation exercises
The alternating motion rate (AMR) task was administered five times in synchronization with a children’s music band song to enhance participant engagement. This involved the sequential repetition of the syllables ‘pa, ta, ka, ra,’ articulated one syllable at a time.
(1) Bite force
Bite force was assessed using the Dental Prescale System II (Fuji Film Co., Tokyo, Japan). To accommodate elderly participants, they were instructed to practice biting several times on thin paper prior to biting the film. Subsequently, participants applied firm occlusion for approximately three seconds to ensure proper placement of the film between the maxillary and mandibular dentition. The films were then retrieved and digitized using a reading scanner, and the maximum bite force was quantified via a bite force analyzer [8]. Improvement in bite force was determined by calculating the difference between post-intervention and pre-intervention measurements, with a greater difference indicating a more substantial enhancement.
(2) Tongue strength
Tongue muscle strength was evaluated using a tongue manometer (Orarize® TPM-02, JMS Co., Ltd., Hiroshima, Japan). Considering the advanced age of the participants, the target pressure was established at 30.0 kPa, reflecting the average tongue pressure observed in individuals aged 65 years and above. Each measurement was conducted three times, with a one-minute interval between trials. The maximum value obtained from these three attempts was recorded as the peak pressure (kPa). Assessment of tongue muscle strength was performed by determining the difference between pre- and post-intervention measurements, where greater values signified enhanced oral muscle function [17].
(3) Maximum mouth opening
Maximum mouth opening (MMO) was quantified as the linear distance between the upper and lower central incisors. This measurement, recorded in millimeters, was obtained using a metal ruler while participants maximally opened their mouths without experiencing pain. Three separate measurements were conducted, each lasting no longer than three seconds, with a 30-second rest interval between trials. The maximum aperture was defined as the mean value of these three measurements [15]. Improvement in maximal aperture was assessed by calculating the difference between pre-intervention and post-intervention values, with a greater difference reflecting enhanced functional capacity.
(4) Articulation alternation movement
The articulation alternation movement test assesses the rapidity with which articulatory movements can be repeated and alternated. Participants were instructed to accurately and sequentially repeat the syllables ‘pa, ta, ka, ra,’ with the number of sequential motion rates (SMR) recorded. While this measure is conventionally obtained over a 5-second interval [13], the present study extended the repetition period to 10 seconds to enhance measurement reliability and mitigate the impact of pronunciation errors, taking into account the reaction speed characteristic of elderly individuals.
If breathlessness was experienced during the measurement, the test was promptly discontinued and subsequently repeated following an adequate rest period. The total score recorded on the paper was transformed into an average number of syllables articulated per second by dividing the total score by ten. This evaluation constitutes an auditory perceptual isometric rating of speech speed and regularity, which is inherently susceptible to rater bias. To mitigate inter-rater variability, the mean value was derived from three repeated measurements. Improvement was assessed by calculating the difference between pre- and postintervention values of articulatory alternation movement, with a greater difference indicating a more effective intervention.
Statistical analyses were performed utilizing IBM SPSS software (version 28.0; IBM Corp., Chicago, IL, USA). The homogeneity of general characteristics, oral health-related variables, and oral muscle functions—including bite force, tongue strength, maximum mouth opening, and articulatory alternating movements—between the experimental and control groups was evaluated using the Chi-square test. Spearman’s correlation analysis was employed to examine the relationships among general characteristics, oral health-related variables, and oral muscle functions. To assess the impact of the oral muscle function exercise program on oral muscle function, repeated measures ANOVA was conducted, with subsequent posthoc analyses applying Bonferroni correction when significant effects were identified.
The uniformity of the general characteristics and oral health-related attributes of the participants was evaluated, indicating no statistically significant differences between the experimental and control groups. Consequently, homogeneity between the two groups was confirmed (p>0.05) <Table 1>.
Table 1. Homogeneity of general and oral health cha racteristics between experimental and control groups
Unit: N(%)
table
*by chi-square test
Exp.: Experimental group; Cont.: Control group
The homogeneity assessment of oral muscle function revealed no statistically significant differences between the two groups in terms of bite force, tongue strength, maximum mouth opening, or articulatory alternation movement, thereby confirming the establishment of homogeneity(p>0.05) <Table 2>.
Table 2. Homogeneity of oral myofunctional characteristics between experimental and control groups
Unit: Mean±SD
table
*by t-test
Exp.: Experimental group; Cont.: Control group
DDK: Diadochokinetic rate
The relationships between general characteristics—such as smoking status, systemic diseases, and medication usage—and oral health-related factors—including denture use, daily brushing frequency, and tongue brushing—were examined in relation to oral muscle function parameters, namely occlusal force, tongue strength, maximum mouth opening, and articulatory alternation. The analysis revealed that the presence of systemic diseases was significantly correlated with both medication use and brushing frequency. Furthermore, a significant association was observed between medication use and brushing frequency. Denture use demonstrated significant associations with bite force, tongue strength, and articulatory alternation. Additionally, bite force showed significant correlations with tongue strength and articulatory alternation <Table 3>.
Table 3. Correlation between general and oral health characteristics and oral myofunction
table
*p<0.05, **p<0.01, ***p<0.001, by Spearman’s rank correlation coefficient
DDK: Diadochokinetic rate
Following the implementation of the oral muscle function exercise program, the experimental group exhibited a notable increase in bite force, with an improvement of 149.66 points. Specifically, bite force values rose from 241.38 points pre-intervention to 292.55 points at 4 weeks and further to 391.04 points at 8 weeks. A significant interaction effect between measurement time and group was observed (p<0.001). Similarly, tongue strength in the experimental group increased by 6.82 points, progressing from 17.48 points before treatment to 20.41 points at 4 weeks and 24.30 points at 8 weeks, with a statistically significant time-by-group interaction (p<0.001). Maximal aperture demonstrated an increase of 0.6 points, from 4.18 points at baseline to 4.35 points at 4 weeks and 4.78 points at 8 weeks, accompanied by a significant interaction between time and group (p<0.001). Furthermore, performance on articulatory alternation exercises improved by 4.85 points in the experimental group, increasing from 13.70 points prior to the program to 15.05 points at 4 weeks and 18.55 points at 8 weeks; this change was also supported by a statistically significant interaction between measurement time and group (p<0.001) <Table 4>.
Table 4. Changes in oral myofunction after performing an oral myofunctional exercise program
Unit: Mean±SD
table
*by Repeated Measures ANOVA
Exp.: Experimental group; Cont.: Control group; G*T: group×time
DDK: Diadochokinetic rate
Sarcopenia is defined as an age-related syndrome marked by the progressive loss of skeletal muscle mass, strength, and physical performance. In 2021, it was formally recognized with the diagnostic code M62.5 in the 8th edition of the Korean Classification of Diseases and Causes of Death (KCD-8) [3]. Preserving and enhancing oral muscle function in older adults is of paramount importance, as diminished oral muscle performance can result in nutritional deficiencies due to impaired mastication, and may contribute to various health complications such as food misdirection, aspiration pneumonia, and halitosis [13,21]. Accordingly, the present study sought to assess the impact of an eight-week oral muscle exercise intervention on the maintenance and improvement of oral muscle function among elderly individuals.
An analysis of general and oral health-related characteristics in relation to oral muscle function revealed a significant association between the presence of systemic diseases, medication usage, and the frequency of daily tooth brushing. This observation is consistent with the findings of Guo et al. [22], who identified that older adults with chronic conditions often exhibit suboptimal oral hygiene practices and encounter difficulties in maintaining oral care, indicating that systemic health status may impact oral hygiene behaviors.
Furthermore, denture use demonstrated a significant correlation with bite force, tongue strength, and articulatory alternation, aligning with the results reported by Komagamine et al. [23], who identified a relationship between tongue and lip motor functions and masticatory performance in individuals wearing complete dentures. These findings imply that these functions are intricately interrelated and constitute essential elements of mastication and oral muscular activity.
In particular, bite force was significantly correlated with tongue strength and articulatory alternation, consistent with the findings of Morita et al. [24], who reported that bite force, tongue strength, and articulatory alternation are closely related to masticatory ability in the elderly.
Following the implementation of the oral muscle function exercise program, significant differences in bite force were observed between groups across different measurement time points. Kashiwazaki et al. [25] demonstrated that gum-chewing exercises administered to elderly participants resulted in a significant increase in bite force post-intervention. In a comparable manner, Hong et al. [6] reported an enhancement in bite force subsequent to bilateral mastication exercises, thereby corroborating the results of the current study.
Significant differences in tongue strength were observed between the experimental and control groups at all measurement intervals. This finding aligns with the results of Kim and Lee’s study [17], which demonstrated notably greater improvements in the cohort that engaged in a combination of calisthenics and tongue strength exercises. Similarly, Bang and Park’s study [26], which utilized the Iowa Oral Performance Instrument (IOPI) to assess tongue pressure, reported increased tongue pressure in the experimental group, corroborating the present study’s outcomes. It is important to note, however, that measurements of tongue pressure may be influenced by the positioning of the device’s bulb, with evidence indicating that posterior tongue pressure tends to be significantly higher than anterior tongue pressure [26]. Consequently, future investigations should carefully consider the placement of the bulb and the selection of measurement instruments. Moreover, it is essential to explore variations in tongue muscle strength not only among healthy elderly populations but also within neurological patient groups. Further research is also warranted to examine the dynamic temporal aspects and movement patterns associated with tongue motility, extending beyond the assessment of static tongue pressure alone.
The maximum aperture size exhibited a significant difference between the experimental and control groups over time, indicating the efficacy of the intervention program. This result is consistent with the findings of Raj et al. [15], who reported an increase in aperture size following oral exercise interventions, as well as those of Lee et al. [21], who observed a similar increase in aperture size within the control group after engaging in oral gymnastics. Maximal opening size is recognized as a critical parameter in oral assessments [21]. In elderly populations, maximal opening size may decline due to various health conditions and alterations in the oral environment. Based on the present study’s findings, it can be concluded that oral muscle function exercise programs have the potential to enhance maximal opening size.
The differences observed between the two groups were statistically significant at all measured time points, thereby substantiating the efficacy of the intervention program. This outcome is consistent with prior research conducted by Morisaki [13], who implemented oral exercises, and Lee et al. [21], who utilized oral gymnastics. Notably, the present study demonstrated a greater enhancement in the speed of articulatory alternation exercises, indicating that harmonica playing may more effectively improve tongue and lip muscle function through repetitive lip and tongue movements. Furthermore, findings from Lee and Kang [20] corroborate these results, as their music therapy program incorporating harmonica playing was shown to enhance oral motor function in stroke patients. Consequently, harmonica playing appears to be a beneficial modality for improving not only articulation but also the oral muscle function of the tongue, lips, and jaw among elderly populations.
This study is subject to several limitations, foremost among them being the small sample size of 37 participants, which constrains the statistical generalizability of the results. Although the oral muscle function exercise program demonstrated efficacy in enhancing oral muscle function over an eight-week duration, the limited participant number diminishes the strength and reliability of the conclusions drawn. Furthermore, despite the utilization of a single-blind design, the potential for rater bias remains, as the researcher was cognizant of group allocations. To address these issues, future research should consider employing a double-blind methodology or implementing measures specifically aimed at reducing rater bias.
Moreover, this study did not account for potential confounding variables, including non-exercise lifestyle factors, nutritional status, and oral hygiene, which may have impacted the findings. To improve internal validity, future research should address these variables either through prior control measures or by incorporating them as covariates in the analysis. Additionally, a more comprehensive assessment of the program’s effectiveness is warranted by implementing it across diverse populations, such as elderly individuals residing in hospitals and nursing care facilities, and by extending the duration of the intervention.
This study holds significance as it empirically examined the impact of an exercise program designed to enhance oral muscle function in elderly individuals aged 65 and above. The intervention incorporated novel methods, including silicone straw biting and harmonica playing, which have not been previously explored in Korean research. Furthermore, by integrating articulation alternation exercises—previously utilized in earlier studies—into children’s music band songs, the program was adapted into an engaging and playful activity that facilitated greater participation among the elderly. This innovative approach not only altered participants’ perceptions regarding oral muscle function but also contributed to its improvement, indicating a potential positive effect on the overall quality of life in this population.
This study sought to assess the efficacy of an oral muscle function exercise regimen in enhancing oral muscle performance among elderly individuals. The intervention was implemented with 20 participants assigned to the experimental group and 17 participants to the control group. The findings from the comparative analysis between these groups are detailed below.
1. Enhancements in bite force, tongue strength, maximum mouth opening, and articulatory movement were observed subsequent to the implementation of the oral muscle function exercise program, relative to baseline measurements obtained prior to the intervention.
2. Analysis of the participants’ articulatory performance indicated that bite force (F=6.201, p<0.01), tongue strength (F=6.953, p<0.01), maximum mouth opening (F=10.592, p<0.001), and articulatory alternation (F=19.394, p<0.001) demonstrated significant enhancements in the experimental group relative to the control group.
The results of this study indicate that the oral muscle function exercise program implemented markedly improves oral muscle function among elderly participants. Therefore, it is essential to explore strategies for incorporating interventions such as silicone straw biting and harmonica playing, alongside conventional oral muscle function exercises, into oral health promotion initiatives within public health centers and eldercare institutions.
Conceptualization: JA Nam; Data collection: JA Nam; Formal analysis: JA Nam; Writing-original draft: JA Nam, AJ Jeong; Writingreview&editing: JA Nam, AJ Jeong, JH Lee
The authors declared no conflicts of interest.
None.
This study was approved by the Institutional Review Board (IRB) of Dong-eui University (IRB No. DIRB-202205-HR-E-10).
Data can be obtained from the corresponding author.
None.