1Department of Preventive Dentistry, School of Dentistry, Kyungpook National University
2Institute for Translational Research in Dentistry, Kyungpook National University
3Department of Dental Technics, Daegu Health College
4Department of Dental Hygiene, Daegu Health College
*The author is a co-first author.
Correspondence to Young-Eun Lee, Department of Dental Hygiene, Daegu Health College, 15 Youngsong-ro, Buk-gu, Daegu-si, 41453, Korea. Tel: +82-53-320-1337, Fax: +82-53-320-1340, E-mail: yelee@dhc.ac.kr
Volume 25, Number 4, Pages 297-310, August 2025.
J Korean Soc Dent Hyg 2025;25(4):297-310. https://doi.org/10.13065/jksdh.2025.25.4.3
Received on June 17, 2025, Revised on July 10, 2025, Accepted on July 25, 2025, Published on August 30, 2025.
Copyright © 2025 Journal of Korean Society of Dental Hygiene.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License(http://creativecommons.org/licenses/by-nc/4.0).
Objectives: Anti-inflammatory dietary patterns and their association with tooth loss remain underexplored, despite extensive research on diet and chronic disease. This study aimed to investigate the association between dietary inflammatory potential and tooth loss due to dental disease. Methods: Data from the 2015-2016 and 2017-March 2020 waves of the United States National Health and Nutrition Examination Survey were analyzed. A total of 3,828 adults aged ≥20 years who underwent oral examinations and provided two days of dietary recall data for the calculation of the Dietary Inflammatory Index (DII), which is a measure of dietary inflammatory potential, were included. Lower DII scores indicate adherence to an anti-inflammatory dietary pattern. Multivariable linear and negative binomial regression models were used for the analyses. Results: Compared with individuals in the lowest DII quintile (indicative of an anti-inflammatory diet), those in the highest quintile (pro-inflammatory diet) exhibited a significantly higher mean ratio (MR) of teeth lost: 1.387 (95% CI: 1.128-1.705). This trend was consistently observed in both the 40–59 and ≥60 years age groups. Conclusions: This study found a significant inverse association between antiinflammatory dietary intake and tooth loss. Targeted dietary counseling and preventive education are essential for reducing the risk of tooth loss in individuals with high consumption of pro-inflammatory nutrients.
Cross-sectional studies, Cytokines, C-reactive protein, Diet, Dietary Inflammatory Index, National Health and Nutrition Examination Survey, Tooth loss
As contemporary society undergoes swift transformation, the determinants of health are increasingly encompassing not only individual lifestyle and environmental factors but also biological influences, health literacy, and the structure of the healthcare system within a community. This has led to an increased focus on oral health, daily nutritional practices, and general systemic well-being. Specifically, socio-economic development and progress in medical technology have led to an enhancement in life expectancy, thereby resulting in a growing elderly population. This demographic transition has subsequently generated considerable apprehensions regarding the quality of life for older individuals [1,2]. Oral health is a critical determinant of quality of life, given its strong correlation with dietary habits. It plays an essential role in overall well-being and is linked to cognitive functioning and the capacity to engage in daily activities [2].
Adequate nutrition derived from dietary consumption is crucial for sustaining life; nevertheless, the prevalence of Westernized dietary patterns—characterized by the intake of processed foods, fast food, convenience items, snacks, and sugary beverages— impedes the consumption of essential fiber, vitamins, and minerals. This may result in increased body weight, disturbances in lipid and energy metabolism, immune system dysfunction, and a range of chronic inflammatory conditions [3]. The Dietary Inflammatory Index (DII), created by Shivappa et al. [4], is a quantitative tool designed to assess the relationship between dietary intake and systemic inflammation. It provides a standardized method to numerically evaluate the inflammatory potential of an individual’s diet. The index operates under the premise that the correlation between six inflammatory blood markers (IL-1β, IL-4, IL-6, IL-10, TNF-α, and C-reactive protein) and particular dietary factors is stable. The DII has been employed to examine correlations with a range of systemic diseases, such as cardiovascular disease [5], metabolic syndrome [6], type 2 diabetes [7], and chronic obstructive pulmonary disease [8]. In the domain of oral health, Kotsakis et al. [9] conducted an analysis utilizing data from the United States National Health and Nutrition Examination Survey (U.S. NHANES) for the years 2009-2010 and 2011-2012. Their findings indicated a correlation between antiinflammatory dietary intake and a decrease in tooth loss. This evidence implies that adopting an anti-inflammatory dietary approach could be a viable public health intervention aimed at preventing oral health issues as well as other systemic inflammatory conditions. In a research study that analyzed data from the 2009-2014 U.S. NHANES, Feng et al. [10] found a significant correlation between dietary patterns characterized by elevated DII scores and the incidence of periodontitis, tooth loss, and indicators of systemic inflammation. Inadequate oral health, stemming from various oral diseases, ultimately culminates in the loss of teeth. Tooth decay and periodontal disease are primary reasons for tooth loss globally. These are prevalent chronic conditions that can impact people of any age. Periodontal disease, especially, tends to increase with age and can lead to tooth loss caused by gingival recession, bleeding, and the destruction of the alveolar bone. Loss of teeth affects chewing ability and can also result in difficulties with speech and problems with the facial and chewing muscles. This issue can complicate eating and may increase the risk of overall malnutrition [11]. Moreover, losing teeth is a major health concern that creates a financial strain not just for individuals, but also for the public health system of a country as a whole. In addition to hindering chewing, losing teeth can negatively impact the grinding, absorption, and digestion of food, which may result in malnutrition. Tooth loss is particularly linked to aging, and its occurrence is on the rise. It has also been noted to have a strong connection with socio-demographic factors [12]. To avoid and lessen tooth loss, it is crucial to implement a dietary approach that reduces chronic inflammation, particularly one that helps ease inflammatory reactions. This method can be seen as an effective way to encourage the adoption of an anti-inflammatory diet in terms of both food choices and nutrition, ultimately improving overall systemic health, including oral health.
To date, few studies have used the DII to evaluate eating habits and their relationship with tooth loss, which is an important aspect of oral health. The U.S. NHANES features a wide variety of ethnic groups and dietary habits, which improves the applicability of the findings regarding the impact of dietary inflammation on the likelihood of tooth loss. This study aimed to determine the association between dietary inflammatory potential and tooth loss due to dental disease, using data from the U.S. NHANES.
This study utilized data from the U.S. NHANES conducted during 2015–2016 and 2017 through March 2020. Adults aged 20 years or older who underwent an oral examination and completed two days of 24-hour dietary recall interviews were eligible for inclusion. Participants were excluded if they provided only one day of dietary recall data (n=2,804), were on unusual diets for health reasons (n=1,780), reported changes in their usual dietary habits (n=3,392), were pregnant or breastfeeding (n=66), or had incomplete data on confounding variables (n=1,489). A total of 3,828 participants were included in the final analysis <Supplementary Fig. S1>. The Institutional Review Board of Kyungpook National University has granted approval for this study (KNU-2025-0209).
The DII was used to evaluate the inflammatory potential of participants’ diets. To construct the DII, Shivappa et al. [4] derived global average intakes and standard deviations for 45 food items from dietary intake data across 11 countries. Furthermore, based on a comprehensive literature review, they assigned each dietary component an Inflammatory Effect score-classified as +1 (proinflammatory), 0 (neutral), or -1 (anti-inflammatory)-according to its association with inflammatory markers.
In this study, the DII was calculated using 28 dietary components, as only these were available from the 24-hour dietary recall data provided by the U.S. NHANES. The DII score can theoretically vary from -5.5 to 5.5 when using 25 to 30 dietary factors. Energy consumption is quantified in kilocalories per day (kcal/day), whereas macronutrients encompass protein (g/day), carbohydrates (g/ day), total fat (g/day), saturated fatty acids (g/day), monounsaturated fatty acids (MUFA; g/day), polyunsaturated fatty acids (PUFA; g/day), cholesterol (mg/day), and dietary fiber (g/day). Micronutrients encompass a variety of essential vitamins and minerals, including vitamin E (mg/day), vitamin C (mg/day), vitamin A (RE/day), beta-carotene (mcg/day), folate (mcg/day), iron (mg/day), magnesium (mg/day), selenium (mcg/day), niacin (mg/day), riboflavin (mg/day), thiamin (mg/day), vitamin B6 (mg/day), vitamin B12 (mcg/day), and zinc (mg/day). Additional nutrients encompass alcohol (g/day), vitamin D (mcg/day), caffeine (mg/day), omega-3 fatty acids (n-3 fatty acids; g/day), and omega-6 fatty acids (n-6 fatty acids; g/day).
The individualized DII was computed in accordance with the methodology established by Shivappa et al. [4]. Initially, we determined the average daily intake by examining two days of dietary data obtained from each participant through the 24-hour dietary recall methodology. Subsequently, we computed the Z-score by subtracting the global average intake from the individual intake of each food parameter and dividing the resultant value by the global standard deviation. Third, we standardized the Z-score to a range between -1 and +1. Fourth, the normalized Z-score was multiplied by the inflammatory effect score associated with each food parameter in order to compute the DII for each individual food item. Ultimately, a personalized DII was developed by aggregating the DII for each of the 28 food parameters. A higher dietary inflammatory index (positive value) signifies a dietary pattern that may facilitate inflammatory responses within the body or affect the biological pathways associated with such responses [4]. Conversely, a low or negative DII signifies a dietary pattern that is characterized by a comparatively elevated consumption of food components linked to anti-inflammatory effects. The DII was classified into quintiles according to the distribution of scores within the study population. The definitions for each quintile are as follows: 1st quintile (Q1; scores less than -0.110), 2nd quintile (Q2; scores ranging from -0.110 to 1.021), 3rd quintile (Q3; scores from 1.022 to 1.948), 4th quintile (Q4; scores from 1.949 to 2.889), and 5th quintile (Q5; scores equal to or greater than 2.890) <Supplementary Fig. S2>.
Oral examinations for the U.S. NHANES were administered by dentists who are licensed to practice in the United States. These professionals have undergone formal education, clinical training, and have successfully completed standardized examination protocols. Oral examinations were conducted in a mobile examination center that included an oral examination room and utilized indirect lighting, a dental mirror, and a periodontal probe. To exclude unintentional tooth loss due to trauma, only cases attributed to dental disease were included in the count of missing teeth.
In order to address potential confounding variables, we incorporated sociodemographic characteristics, body mass index (BMI), health-related behaviors, and chronic disease indicators into our analysis. Demographic characteristics included age categories (20–39, 40–59, ≥60 years), sex, race/ethnicity (non-Hispanic White, non-Hispanic Black, Asian, other non-Hispanic, Mexican American, other Hispanic), education level (middle school or below, high school, some college or above), income level (low, moderate, or high, based on household poverty thresholds), and marital status (never married, married or living with partner, divorced, separated, or widowed). BMI was categorized as normal or underweight (≤24.9 kg/m²), overweight (25.0–29.9 kg/m²), and obese (≥30.0 kg/m²) [13]. Health-related behaviors included smoking status (never smoker, former smoker consuming <10 or ≥10 cigarettes per day, occasional smoker, and daily smoker) and physical activity level (inactive, inadequately active, active, and highly active). Hypertension was defined as having a mean systolic/diastolic blood pressure of ≥130/80 mmHg or the use of antihypertensive medications [14]. Diabetes was identified based on at least one of the following: a previous diagnosis, fasting glucose ≥126 mg/dL, glycated hemoglobin (HbA1c) ≥6.5%, or the use of antidiabetic medications [15].
A multivariable linear regression analysis was performed to investigate the association between the DII and tooth loss. The unstandardized coefficient (β) along with the 95% confidence interval (CI) were computed to assess statistical significance. A negative binomial regression model was employed to assess the risk of tooth loss across the quintiles of the DII. The mean ratio (MR) and the 95% CI for the average number of teeth lost were computed. Weights were assigned to participants in the two-day 24-hour dietary recall interview (WTDR2D) and were subsequently adjusted through post-stratification based on sex, age, and race/ethnicity, in accordance with population estimates provided by the U.S. Census Bureau. Integrated weights from multiple survey cycles were then calculated and applied to the analysis. All statistical analyses were performed using R version 4.4.2 (R Foundation for Statistical Computing, Vienna, Austria), with a significance level of 0.05.
Among 3,828 participants, 1,166 individuals (36.1%) were within the age range of 20 to 39 years, 1,253 individuals (34.8%) were aged between 40 and 59 years, and 1,409 individuals (29.1%) were aged 60 years or older. The sex distribution consisted of 2,111 males, representing 48.1% of the total, and 1,717 females, accounting for 51.9%. In terms of race and ethnicity, non-Hispanic whites represented the highest proportion, accounting for 64.2%. Regarding educational level, 67.2% of individuals possessed a college degree or a higher qualification. Additionally, 47.7% indicated a high income, while 63.6% were either married or living in a cohabiting arrangement. According to classifications based on BMI, 38.8% of the population was identified as obese, 32.4% as overweight, and 28.8% as either of normal weight or underweight. Regarding health behaviors, the engagement in regular physical activity was the most frequently reported, with 59.6% of participants indicating participation. Conversely, the most commonly reported smoking status was noted at 56.4%. The prevalence rates were 46.0% for hypertension and 11.3% for diabetes. The mean total of natural teeth present was 23.84, whereas the mean number of teeth lost due to dental disease was 3.76 <Table 1>. In the highest quintile of the DII (the upper 20%), the principal nutrients associated with pro-inflammatory effects included dietary fiber (+0.594), beta-carotene (+0.500), vitamin E (+0.415), vitamin D (+0.376), and vitamin C (+0.367) <Fig. 1>.
Table 1. General characteristics of the study participants
table
N: unweighted frequency; %: weighted percentage; Mean: weighted mean; SD: standard deviation
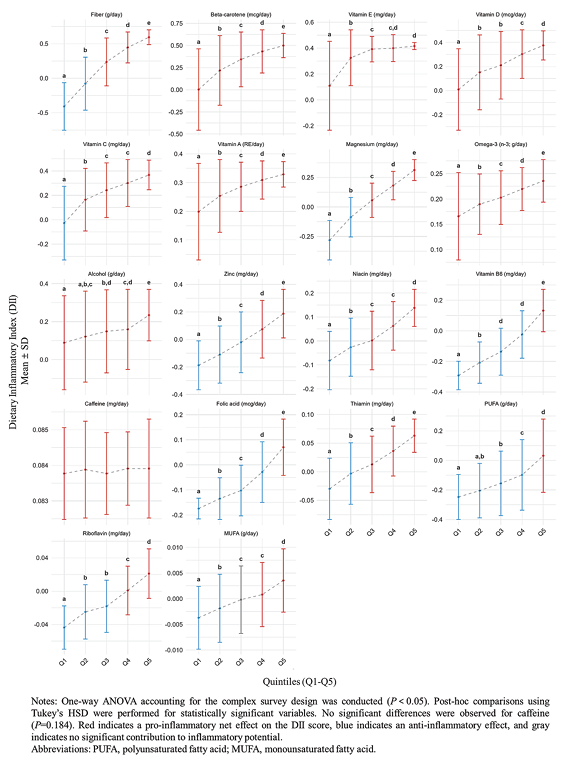
Fig. 1. Distribution of nutrients with the positive impact on Dietary Inflammatory Index in the highest quintile group (Q5)
Multivariable linear regression analysis demonstrated that an increased DII score was significantly associated with greater tooth loss due to dental disease, even after adjusting for confounders (β=0.275; 95% CI: 0.131–0.418; p=0.001) <Table 2>.
Table 2. Linear regression analysis of the association between Dietary Inflammatory Index and tooth loss
table
Multivariable linear regression was conducted accounting for the complex survey design (p<0.05).
*adjusted for age, sex, race/ethnicity, education level, income level, marital status, body mass index
†adjusted for age, sex, race/ethnicity, education level, income level, marital status, body mass index, smoking status, physical activity level, hypertension, and diabetes
β: unstandardized coefficient; CI: confidence interval
Negative binomial regression analysis indicated that the mean number of teeth lost increased progressively across higher quintiles of the DII, even after adjusting for confounders. Specifically, the adjusted MRs of tooth loss due to dental disease were 1.149 (95% CI: 0.923–1.429; p=0.191) for the third quintile, 1.224 (95% CI: 0.928–1.614; p=0.136) for the fourth quintile, and 1.387 (95% CI: 1.1281.705; p=0.005) for the fifth quintile <Table 3>. In the age-stratified subgroup analysis, no significant differences were observed across DII quintiles among participants aged 20–39 years. However, significant differences were observed among participants aged 40–59 years and those aged ≥60 years. Compared to participants in the first DII quintile, those in the fifth quintile had adjusted MRs of tooth loss of 1.646 (95% CI: 1.025–2.643; p=0.041) for the 40–59 age group and 1.322 (95% CI: 1.010–1.731; p=0.043) for the ≥60 age group, respectively <Table 4>.
Table 3. Mean ratios for tooth loss according to Dietary Inflammatory Index quintiles (Q1–Q5)
table
Negative binomial regression was conducted accounting for the complex survey design (p<0.05).
*adjusted for age, sex, race/ethnicity, education level, income level, marital status, body mass index
†adjusted for age, sex, race/ethnicity, education level, income level, marital status, body mass index, smoking status, physical activity level, hypertension, and diabetes
MR: mean ratio; CI: confidence interval
Table 4. Mean ratios for tooth loss according to Dietary Inflammatory Index quintiles (Q1–Q5) by age group
table
Negative binomial regression was conducted accounting for the complex survey design (p<0.05).
*adjusted for age, sex, race/ethnicity, education level, income level, marital status, body mass index
†adjusted for age, sex, race/ethnicity, education level, income level, marital status, body mass index, smoking status, physical activity level, hypertension, and diabetes
MR: mean ratio; CI: confidence interval
This study aimed to explore the association between dietary inflammatory potential and tooth loss due to dental disease. The results showed that participants in the most pro-inflammatory diet group (DII quintile 5) had a significantly greater mean number of teeth lost compared to those in the most anti-inflammatory diet group (DII quintile 1). This trend was consistently observed in both the 40–59 and ≥60 age groups. These findings suggest that a higher dietary inflammatory potential is associated with an increased risk of tooth loss in middle-aged and older adults.
Beta-carotene, vitamin E, and vitamin D-all known for their anti-inflammatory properties-were consistently consumed at inadequate levels across all DII quintiles (Q1-Q5), which contributed to elevated DII scores <Fig. 1>. Beta-carotene, a carotenoid and natural pigment found in numerous fruits and vegetables, is recognized for its ability to modulate systemic inflammatory responses, which can be ascribed to its antioxidant and anti-inflammatory properties. A significant decrease in serum C-reactive protein levels has been observed in individuals following a diet rich in beta-carotene [16]. Vitamin E is found in a variety of plant-based foods, including cooking oils, almonds, spinach, and broccoli. It is acknowledged as one of the most essential fat-soluble antioxidants that contribute to the maintenance of homeostasis within the body [17]. A meta-analysis suggests that α-tocopherol is the most bioactive form of vitamin E. Additionally, a daily supplementation of 500 mg or more has been statistically associated with an average reduction in C-reactive protein levels of 0.52 mg/L [18]. Although the exact mechanism by which vitamin D operates is not fully understood, current research suggests that it has a variety of regulatory effects on both the innate and adaptive immune systems [19]. Research has demonstrated that elevated inflammation associated with insufficient magnesium intake has been observed across various tertiles. A retrospective cohort study conducted among U.S. adults identified a relationship between low magnesium consumption and elevated levels of inflammatory markers, including high-sensitivity C-reactive protein, which is implicated in the development of systemic inflammation and metabolic disorders [20]. Moreover, heightened inflammation levels linked to insufficient zinc intake were observed across various quintiles <Fig. 1>. Zinc is essential for the regulation of cellular proliferation and differentiation, and the immune system, which relies heavily on effective cellular proliferation, is particularly susceptible to zinc deficiencies [21]. The DII is predicated on the hypothesis that six inflammatory biomarkers present in the bloodstream-specifically IL-1β, IL-4, IL-6, IL-10, TNF-α, and C-reactive protein-exhibit interconnections [4]. This interrelationship suggests that chronic systemic inflammation, which may result from a diet deficient in anti-inflammatory components, could contribute to the incidence of tooth loss.
By categorizing the DII into quintiles and analyzing the contribution of individual dietary components, we found that the increase in DII was primarily attributable to the inadequate intake of anti-inflammatory nutrients <Fig. 1>. Inadequate management of systemic inflammation via a suitable anti-inflammatory diet may compromise immune responses to periodontopathogenic bacteria, thereby increasing the likelihood of tooth loss. Middle-aged Americans, particularly those aged 45 to 64 years, demonstrate the highest prevalence of severe periodontitis and are at a heightened risk for tooth loss [22]. Periodontitis has the potential to induce systemic inflammation via various mechanisms. Instances encompass the hematogenous dissemination of periodontal pathogens and inflammatory mediators, in addition to the systemic migration of activated lymphocytes [23]. This form of persistent low-grade inflammation is acknowledged as a significant contributor to the onset of several metabolic disorders. Type 2 diabetes mellitus, which is characterized by the development of insulin resistance, adversely affects the cellular repair mechanisms that respond to damage inflicted by subgingival bacteria. This dysfunction is linked to increased concentrations of inflammatory cytokines, such as interleukin-1β and interleukin-6, in addition to elevated levels of C-reactive protein, a marker indicative of acute-phase inflammation. Consequently, the persistent accumulation of low-grade chronic inflammation may ultimately result in the loss of teeth [24]. Furthermore, visceral fat, which plays a crucial role in the development of abdominal obesity, secretes inflammatory adipokines such as tumor necrosis factor-α and interleukin-6 [25]. These molecules are recognized for their ability to disturb metabolic equilibrium and intensify low-grade chronic inflammation. Tooth loss is commonly noted among individuals exhibiting abdominal obesity [26], indicating that chronic inflammation associated with metabolic dysregulation may intensify periodontal inflammation, thereby contributing to the loss of teeth. The mitigation and management of systemic inflammation are essential for the prevention of metabolic disorders and the reduction of the likelihood of tooth loss. Consequently, adhering to an anti-inflammatory diet is crucial for reducing systemic inflammation and preserving metabolic equilibrium.
Research indicates that around 21% of American adults between the ages of 20 and 64 have untreated dental caries [27], whereas a significant 96% of individuals aged 65 and older have encountered dental caries at some point in their lives [28]. Tooth loss attributable to dental disease, as delineated in this research, encompasses loss resulting from dental caries, which may possess limited efficacy as a mediator of systemic inflammation. By analyzing the diverse characteristics of anti-inflammatory foods, it is possible to ascertain their potential advantages. The dietary component exhibiting the lowest consumption within the quintile of the DII was dietary fiber <Fig. 1>. Dietary fiberis present in whole grains, vegetables, and fruits, promotes the self-cleaning effect in the oral cavity and provides various micronutrients essential for maintaining oral health. Research conducted on adults in the United States has identified a relationship between insufficient dietary fiber consumption and a heightened risk of dental caries [29]. Consequently, it is imperative to prioritize sufficient fiber consumption as a means of enhancing dietary practices aimed at preventing tooth loss.
This study’s strengths include the use of nationally representative data, which ensures external validity through post-stratification adjustments and survey weighting. Moreover, subgroup analyses considering age-related differences in tooth loss were conducted, enabling more detailed and robust findings through complex statistical approaches. Despite these strengths, this study has certain limitations. First, the DII assesses the inflammatory potential of nutrients but does not fully capture dietary patterns, including food types and processing levels. Further analysis considering these factors is needed. Second, this research employed only 28 out of the 45 available items to compute the DII, thereby constraining the interpretation of the findings. Third, a two-day period of 24-hour dietary recall may not provide a comprehensive representation of an individual’s overall dietary consumption. Nevertheless, by omitting participants whose dietary consumption may have been affected and implementing a weighting adjustment that accounted for the day of the week and non-response (WTDR2D), we improved the robustness of our results. Fourth, tooth loss due to other causes was not considered in this study. Subsequent research should incorporate a more comprehensive array of factors that influence tooth loss. Fifth, this research is grounded in data from the U.S., its findings may have limited generalizability to the dietary patterns and cultural characteristics specific to Korea. Nonetheless, the principal benefit of employing U.S. data lies in its representation of a wide range of ethnicities, dietary practices, and cultural contexts. This diversity facilitates a more comprehensive assessment of the hypothesis concerning the association between dietary inflammation and tooth loss. Future research endeavors should include data from Korea. Furthermore, by conducting comparative analyses of the findings from this study alongside data from both the United States and Korea, researchers will be able to evaluate the influence of ethnic and cultural variables on the association between anti-inflammatory dietary consumption and tooth loss attributable to dental disease.
This study aimed to examine the association between dietary inflammatory potential and tooth loss due to dental disease, using data from the U.S. NHANES.
1. A progressive increase in the mean number of teeth lost was observed across DII quintiles. Participants in the most proinflammatory diet group (DII quintile 5) exhibited a mean tooth loss that was 1.387 times as high as those in the most antiinflammatory diet group (DII quintile 1).
2. Age-stratified subgroup analysis revealed that within the 40–59 and ≥60 age groups, participants in the most pro-inflammatory diet group (DII quintile 5) had mean tooth losses 1.646 and 1.322 times as high, respectively, as those in the most anti-inflammatory diet group (DII quintile 1).
In middle-aged and older adults, inadequate consumption of anti-inflammatory dietary components has been associated with an increased risk of tooth loss due to dental disease. This underscores the importance of dietary recommendations and preventive education for individuals who consume a high quantity of pro-inflammatory foods, as these measures may contribute to a decreased risk of tooth loss.
Conceptualization: YJ Lee, YE Lee; Data collection: YJ Lee, HJ Go; Formal analysis: YJ Lee, HJ Go; Writing-original draft: YJ Lee, HJ Go, YE Lee; Writing-review&editing: YJ Lee, HJ Go, JM Kang, YE Lee
YE Lee is a member of the Editorial Committee of the Journal of the Korean Society of Dental Hygiene, but was not involved in the review process of this manuscript. The authors declare no other conflicts of interest.
None.
The study was approved as exempt by the Kyungpook National University Institutional Review Board (KNU-2025-0209) for secondary analysis of de-identified U.S. NHANES data.
The U.S. NHANES data files used in this study are publicly available on the official website, provided by the Centers for Disease Control and Prevention.
We gratefully acknowledge Professor Emeritus Keun-Bae Song of the Department of Preventive Dentistry, Kyungpook National University, School of Dentistry, for his valuable review and insightful comments on the manuscript.