1Department of Dental Hygiene, Ansan University
2Department of Dental Hygiene, Hanyang Women’s University
Correspondence to Kyung-Hwa Park, Department of Dental Hygiene, Hanyang Women’s University, 200 Salgoji-gil, Seongdong-gu, Seoul-si, Korea. Tel: +82-2-2290-2570, Fax: +82-2-2297-3867, E-mail: pkh2735@hanmail.net
Volume 25, Number 4, Pages 311-21, August 2025.
J Korean Soc Dent Hyg 2025;25(4):311-21. https://doi.org/10.13065/jksdh.2025.25.4.4
Received on July 08, 2025, Revised on July 21, 2025, Accepted on August 04, 2025, Published on August 30, 2025.
Copyright © 2025 Journal of Korean Society of Dental Hygiene.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License(http://creativecommons.org/licenses/by-nc/4.0).
Objectives: The aim of this study was to examine the association between substance use and oral symptoms among Korean adolescents. Methods: A secondary data analysis was conducted using raw data from the 2024 Korean Youth Risk Behavior Survey administered by the Korea Disease Control and Prevention Agency (KDCA). A total of 53,166 adolescents with no missing data were included in the analysis. Multivariate logistic regression was performed after adjusting for potential confounders. Results: After adjusting for confounding variables, adolescents with a history of substance use were 1.28 times more likely to report tooth pain or throbbing and 1.51 times more likely to report gum pain or bleeding than those with no history of substance use. Conclusions: Substance use during adolescence was significantly associated with adverse oral symptoms. These findings highlight the need for substance use prevention programs, oral health education tailored to adolescents. and active governmentlevel policy interventions to address this growing public health concern.
Adolescents, Oral health, Oral symptoms, Substance use experience
Adolescence constitutes a developmental stage characterized by significant physiological and psychological transformations, during which substance use emerges as a critical global public health issue [1]. The ramifications of adolescent substance use extend beyond individual health, contributing to extensive societal challenges [1]. Recent epidemiological data reveal that the lifetime prevalence of habitual and intentional drug consumption among adolescents was estimated at 1.6% in 2022 (1.5% among males and 1.8% among females), 1.7% in 2023 (1.5% among males and 1.8% among females), and 1.4% (1.2% among males and 1.6% among females) for substances including tranquilizers, stimulants, hypnotics, appetite suppressants, narcotic analgesics, and inhalants such as glue, cannabis, cocaine, or butane gas [2]. These prevalence rates indicate an upward trend relative to prepandemic levels, accompanied by exacerbated adverse health outcomes [3]. The etiology of adolescent drug use is multifactorial, encompassing familial influences, peer interactions, socioeconomic factors, and systemic health determinants. Access to these substances is frequently facilitated through interpersonal networks involving adults, peers, or older adolescents, with a growing proportion obtained via online platforms [4–6].
Dental caries is manifested by symptoms such as toothache, halitosis, and periodontal disease. Periodontal disease often initiates with mild clinical signs, including gingival bleeding or gingivitis. Due to the subtle nature of early-stage symptoms, which are frequently overlooked, timely intervention is often missed [7]. Once established, these oral pathologies are challenging to reverse, underscoring the importance of preventive measures to maintain oral health [8]. Recent epidemiological data indicate that the prevalence of permanent dental caries among 12-year-old individuals is 60.3%, with a permanent caries index of 1.9. This reflects a 1.9% increase in caries prevalence between 2021 and 2022. Furthermore, the incidence of gingival pain and bleeding has reached 39.8%, representing a 50% rise over the same period [9]. The oral health status of adolescents plays a critical role in determining their oral health outcomes in adulthood, necessitating proactive support from both individuals and governmental bodies at national and local levels.
Substance abuse is associated with significant oral health complications, including dental caries, periodontal disease, mucosal dysplasia, xerostomia, bruxism, dental attrition, and tooth loss [10]. The incidence of dental caries, periodontal disease, and xerostomia is notably elevated among individuals diagnosed with substance use disorders. The use of illicit drugs directly induces xerostomia, which in turn heightens vulnerability to dental caries [11]. Adolescence represents a critical developmental phase characterized by unique gut and oral microbiome compositions distinct from other life stages [12]. During this period, the microbiome exhibits heightened sensitivity to various substances such as alcohol, nicotine, opioids, and amphetamines, leading to dysbiosis marked by the predominance or depletion of specific microbial taxa. These microbiome alterations are intricately linked to physical and immune system development, as well as an increased susceptibility to the effects of substance use [12].
Recent investigations into adolescent substance use have examined alterations in usage patterns, the prevalence of substance use experiences, contributing factors, correlations between physical activity and healthcare behaviors, as well as associations with suicidal ideation, alcohol consumption, and tobacco use [3–5,13–15]. Nonetheless, research specifically addressing oral health within this context remains scarce. A limited number of studies have explored the linkage between health risk behaviors and oral symptomatology among adolescents from multicultural backgrounds [8,16,17], alongside analyses of the relationships among depressive symptoms, suicidal ideation, and oral health complaints in middle and high school populations [8,16,17]. For instance, Park and Lee [8] identified a higher incidence of oral symptoms—such as tooth pain during mastication, persistent toothache, and gingival soreness or bleeding—among habitual drug users relative to non-users. Conversely, Sim and Hong [17] reported no statistically significant association between drug use and oral symptoms, including tooth pain, gum discomfort, and halitosis. In light of these divergent findings, the present study seeks to elucidate whether drug use, recognized as a health risk factor, exerts a direct influence on oral health outcomes.
This study examines the relationship between oral symptoms and substance use in adolescents with a history of substance consumption, thereby establishing a basis for the formulation of policies and the implementation of effective preventive education programs designed to mitigate substance use and enhance oral health in this population.
This research employed primary data obtained from the 2024 Youth Health Behavior Survey, a collaborative effort between the Korea Centers for Disease Control and Prevention and the Ministry of Education, authorized by the National Statistical Office (Approval No. 117058). The analysis was conducted using a complex sampling framework that accounted for stratification, clustering, weighting, and finite population correction. The study sample comprised 54,653 individuals, among whom 53,166 provided responses to items concerning lifetime habitual and intentional drug use, oral health symptoms (such as tooth pain during eating, toothache, throbbing sensations, and sore or bleeding gums), as well as demographic and behavioral variables including gender, grade level, academic achievement, living arrangements, household economic status, alcohol consumption, smoking habits, physical activity, obesity status, frequency of daily tooth brushing, perceived stress, depression, and suicidal ideation <Fig. 1>.
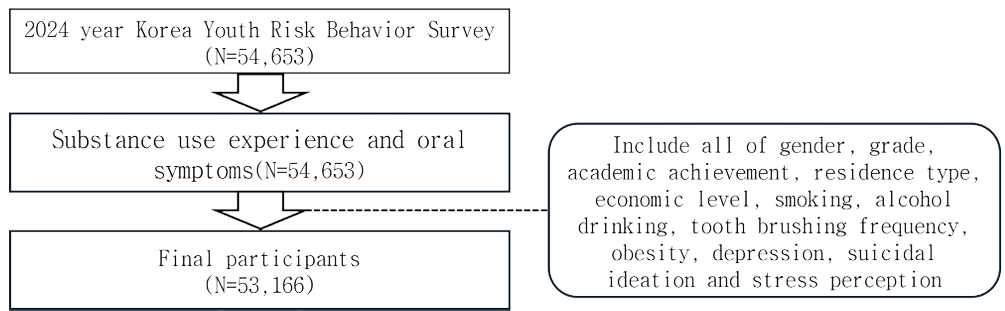
Fig. 1. Flow of study
Gender was classified into two categories: ‘male’ and ‘female’. Grade level was categorized as either ‘middle school’ or ‘high school’. Living arrangements were divided into ‘living with family’ and ‘living with others’. Academic performance and family economic status were each stratified into three levels: ‘high’, ‘medium’, and ‘low’. Health behavior variables were dichotomized as follows: lifetime alcohol consumption was recorded as ‘yes’ or ‘no’; smoking status for conventional tobacco (cigarettes), cigarettelike e-cigarettes, and nicotine-containing liquid e-cigarettes was categorized as ‘never’ or ‘yes’; and engagement in vigorous physical activity for 60 minutes or more within the past seven days was classified as ‘yes’ or ‘no’. Oral health behaviors were categorized based on frequency of tooth brushing, distinguishing between brushing less than twice per day and brushing two or more times per day.
Obesity was assessed using the body mass index (BMI), calculated as body weight in kilograms divided by the square of height in meters [BMI=body weight (kg) / [height (m)]2]. Based on established criteria [19], individuals with a BMI below 25 kg/m² were classified as ‘normal,’ whereas those with a BMI exceeding 25 kg/m² were categorized as ‘obese’. Habitual and intentional drug use was defined as affirmative if participants reported any prior use of substances including visual stabilizers, stimulants, hypnotics, appetite suppressants, narcotic analgesics, or consumption of substances such as bonds, cannabis, cocaine, or butane gas. Oral health symptoms were dichotomized as ‘never’ or ‘yes’ depending on whether participants had experienced any of the following within the preceding 12 months: tooth pain triggered by consumption of cold or hot foods or beverages; tooth pain during eating; toothache characterized by throbbing or general dental pain; and sore or gingival bleeding.
The present study utilized IBM SPSS Statistics software (version 22.0; SPSS Inc., Chicago, IL, USA) to analyze raw data obtained from the 2024 Youth Health Behavior Survey. Variations in oral symptoms relative to participants’ general characteristics, as well as differences in drug use experience based on these characteristics, were investigated through composite sample crosstabulation analysis. Furthermore, the relationship between drug use experience and oral symptoms was evaluated using composite sample logistic regression analysis, with variables demonstrating significant differences in oral symptoms according to general characteristics included as confounding factors. The statistical significance level was set at 0.05.
<Table 1> presents the analysis of variations in oral symptoms based on the general characteristics of the study participants. Female subjects reported a higher prevalence of oral symptoms compared to their male counterparts. Participants with lower family economic status exhibited a greater likelihood of experiencing oral symptoms relative to those with higher economic status. Additionally, individuals who engaged in smoking or alcohol consumption were more prone to report oral symptoms than nonusers. Participants who brushed their teeth fewer than twice daily demonstrated a higher incidence of symptoms compared to those who brushed more frequently. The perception of stress was also associated with an increased reporting of oral symptoms. Furthermore, individuals with a history of drug use reported a higher frequency of symptoms than those without such history. Participants diagnosed with depression and those experiencing suicidal ideation reported significantly more oral symptoms than their respective counterparts (p<0.001). High school students were more likely than middle school students to report toothache and throbbing pain (p<0.001). Moreover, lower academic performance was more prevalent among participants who engaged in physical activity compared to those who did not (p<0.001).
<Table 2> presents the variations in drug use experience based on the general characteristics of the study population. Female participants exhibited a higher likelihood of drug use compared to their male counterparts. Additionally, high school students demonstrated a greater propensity for drug use relative to middle school students. The prevalence of drug use showed an increasing trend corresponding to academic performance and family economic status, ranked from ‘middle’ to ‘upper’ to ‘lower’. Concerning living arrangements, individuals residing with others were more prone to drug use than those living with family members. Moreover, participants who engaged in smoking, alcohol consumption, or physical activity were more likely to have used drugs than those who did not partake in these behaviors. Drug use prevalence was also elevated among individuals who brushed their teeth fewer than twice daily compared to those who maintained oral hygiene more frequently. Finally, the incidence of perceived stress, depression, and suicidal ideation was significantly greater among individuals reporting these conditions than among those without such experiences (p<0.05).
Table 1. Distribution of oral symptoms by general characteristics of participants
(N=53,166)
table
Values are presented as unweighted number and weighted %.
*by complex samples chi-square test
Table 2. Substance use experience according to general characteristics of the study subjects
(N=53,166)
table
Values are presented as unweighted number and weighted %.
*by complex samples chi-square test
<Table 3> illustrates the relationship between substance use history and oral health symptoms. Controlling for variables including gender, grade level, academic achievement, household economic status, smoking, alcohol consumption, physical activity, daily tooth brushing frequency, perceived stress, depression, and suicidal ideation, individuals with a history of drug use exhibited a 1.28fold increased risk of experiencing toothache and throbbing pain compared to those without such a history. Likewise, after adjusting for gender, living arrangement, household economic status, smoking, alcohol consumption, physical activity, daily tooth brushing frequency, perceived stress, depression, and suicidal ideation, the likelihood of reporting sore or bleeding gums was 1.51 times greater among individuals who had ever used drugs relative to those who had never used drugs.
Table 3. Association between oral symptoms and substance use experience
table
Values were estimated odds ratio (95% confidence interval).
* by complex sample multivariate logistics regression
1)multivariable includes gender, economic level, smoking, alcohol drinking, tooth brushing frequency, stress perception, depression, suicidal ideation
2)multivariable includes gender, grade, academic achievement, economic level, smoking, alcohol drinking, physical activity, tooth brushing frequency, stress perception, depression, suicidal ideation
3)multivariable includes gender, residence type, economic level, smoking, alcohol drinking, tooth brushing frequency, stress perception, depression, suicidal ideation
This study employed raw data from the 20th Youth Health Behavior Survey (2024) to investigate the relationship between substance use experience and oral health symptoms among Korean adolescents. Analysis of variations in oral symptoms according to the general characteristics of the participants revealed that the occurrence of tooth pain during eating differed significantly by gender, household economic status, smoking behavior, alcohol consumption, frequency of daily tooth brushing, perceived stress levels, and substance use experience. Additionally, the prevalence of toothache and throbbing pain varied across groups defined by gender, grade level, academic achievement, household economic status, smoking, alcohol use, physical activity, daily brushing frequency, perceived stress, and substance use experience. Regarding symptoms of sore or bleeding gums, significant differences were identified based on gender, living arrangements, household economic status, smoking, alcohol consumption, physical activity, brushing frequency, perceived stress, and drug use. These results align with findings reported in previous studies by Moon et al. [20], Bae et al. [21], and Kim and Lim [22].
This study identified variations in the experience of oral symptoms that correlate with demographic factors, mental health status, lifestyle choices, oral health behaviors, and health risk indicators. These results underscore the necessity for tailored oral health education programs within schools, alongside enhanced institutional support, to effectively improve the oral health outcomes of adolescents.
Furthermore, analysis of substance use experiences revealed significant differences associated with participants’ general characteristics, including gender, grade level, academic achievement, living arrangements, household economic status, smoking habits, alcohol consumption, physical activity, frequency of daily tooth brushing, perceived stress, depression, and suicidal ideation. These findings suggest that substance use behaviors are influenced by a complex interplay of socioeconomic conditions, healthrelated behaviors, oral hygiene practices, and mental health factors. Such results align with prior research conducted by Lee and Lee [3] and Baeck and Kim [4], thereby reinforcing the reliability and validity of the present study’s conclusions.
Extensive research has demonstrated that academic and economic instability, coupled with insufficient familial support, significantly contribute to substance use. Such unstable conditions engender psychological stress among adolescents, thereby elevating their susceptibility to a range of maladaptive behaviors, notably alcohol and substance use disorders [4]. Furthermore, peer relationships play a pivotal role during adolescence, underscoring the importance of implementing after-school programs designed to foster positive peer interactions and enhance youths’ sense of achievement.
Concerning the relationship between drug use history and oral health symptoms, after controlling for potential confounders, individuals with a history of drug use exhibited a 1.28-fold increased likelihood (95% CI: 1.09–1.50) of experiencing toothache and throbbing pain, as well as a 1.51-fold increased likelihood (95% CI: 1.26–1.80) of reporting sore or bleeding gums, relative to those who had never used drugs. Choi and Lee [16] documented a 0.53-fold lower prevalence of oral disease symptoms among individuals without habitual drug use. In a similar vein, Park and Lee [8] identified a higher prevalence of oral symptoms among habitual drug users compared to non-users, with odds ratios of 1.235 for tooth pain during mastication, 1.579 for toothache and throbbing, and 1.512 for sore or bleeding gums. These findings corroborate the results observed in the current study.
Sim and Hong [17] conducted a study involving adolescents from multicultural families, which identified differences in gum pain and halitosis between individuals with and without substance use. However, their risk assessment did not demonstrate a statistically significant association, a finding that diverges from the results of the present study. This discrepancy may be explained by the temporal context of their data collection, which occurred prior to the COVID-19 pandemic. During that period, the prevalence of medication use remained relatively stable, recorded at 0.5% in 2016, 0.6% in 2017, 0.5% in 2018, and 0.5% in 2019 [2]. In contrast, data collected following the onset of the COVID-19 pandemic indicate an increase in prevalence to 1.6% in 2022, 1.7% in 2023, and 1.4% in 2024 [2].
Oral complications associated with the use of illicit substances encompass dental caries, periodontitis, tooth loss, and compromised oral hygiene [23]. Clinical manifestations such as dental pain, pulsating discomfort, and inflamed or bleeding gingiva are indicative of underlying dental decay and periodontal pathology. Although these conditions may remain asymptomatic during initial stages, they have the potential to advance to dentoalveolar bone degradation, ultimately necessitating tooth extraction. The nature and severity of oral health issues related to substance abuse are influenced by the specific drug involved and its route of administration, including direct contact with oral tissues via oral, intravenous, or inhalational pathways, the chemical properties of the substance, and drug-induced modifications in salivary pH levels [24]. Furthermore, substance use can impair cognitive functioning, which adversely affects individuals’ behaviors and attitudes toward oral hygiene maintenance [25].
During adolescence, the prefrontal cortex remains underdeveloped, which contributes to increased impulsivity and heightened sensitivity. Exposure to substances during this critical developmental window can disrupt the maturation of the prefrontal cortex, thereby elevating the long-term risk of addiction [26]. The lifestyle behaviors and experiences acquired during adolescence exert a profound influence on an individual’s trajectory, as these patterns frequently persist into adulthood. Specifically, a history of substance use during this period is associated with a greater propensity for developing drug addiction, resulting in sustained substance use later in life. Additionally, oral health practices established during adolescence not only affect oral health outcomes in adulthood but also play a crucial role in shaping knowledge and attitudes regarding oral health.
Understanding substance use behaviors among adolescents necessitates an examination of multiple interacting factors, particularly the social environments in which they reside. Existing research has demonstrated a significant association between substance use and oral health symptoms. Consequently, the development of an integrated collaborative framework involving school counselors, dental hygienists, and community health centers is imperative to facilitate preventive education. Moreover, proactive governmental involvement is essential in addressing this issue.
The present study utilized a cross-sectional design, which inherently restricts the capacity to establish causal inferences. Furthermore, given the strong relationship between oral symptoms and dietary intake, the absence of dietary data in the analysis represents a limitation. Future investigations should incorporate dietary variables to provide a more comprehensive understanding of the factors influencing oral health in the context of adolescent substance use.
This study employed raw data from the 2024 National Youth Health Behavior Survey conducted by the Korean Centers for Disease Control and Prevention to investigate the relationship between substance use experience and oral health symptoms among adolescents.
1. Variations in oral symptoms according to the general characteristics of the study participants revealed that tooth pain experienced during food consumption differed significantly by gender, household economic status, smoking habits, alcohol use, frequency of daily tooth brushing, perceived stress levels, history of medication use, presence of depression, and suicidal ideation. Similarly, the occurrence of throbbing or aching tooth pain was associated with differences across gender, academic grade, academic performance, household economic status, smoking, alcohol consumption, physical activity, daily tooth brushing frequency, perceived stress, medication use history, depression, and suicidal thoughts. Furthermore, the incidence of gum pain or bleeding demonstrated significant variation based on gender, type of residence, household economic status, smoking, alcohol consumption, frequency of tooth brushing per day, perceived stress, medication use experience, depression, and suicidal ideation.
2. Variations in substance use experience were observed based on substance type, household economic status, smoking behavior, alcohol consumption, frequency of daily tooth brushing, physical activity levels, perceived stress, depression, and other demographic characteristics of the study population. Furthermore, substance use experience differed significantly according to gender, academic grade, academic achievement, and the presence of suicidal ideation among participants.
3. In examining the relationship between substance use and oral health symptoms, after controlling for potential confounding factors, individuals with a history of substance use exhibited a 1.28-fold increased likelihood of experiencing toothache and throbbing pain, and a 1.51-fold increased likelihood of reporting sore or bleeding gums compared to those without such history.
The findings of this study demonstrate a significant association between adolescents’ substance use experience and the occurrence of oral symptoms. Consequently, to effectively prevent habitual and intentional drug use among this population and to enhance oral health outcomes, a comprehensive strategy encompassing oral health education, lifestyle modifications, and structured preventive programs is essential.
Conceptualization: KH Park; Data collection: KH Park; Formal analysis; KH Park; Writing-original draft; KH Park, SK Jun; Writingreview & editing: KH Park, SK Jun
The authors declared no conflicts of interest.
None.
None.
Data can be obtained from the corresponding author.
None.