Department of Dental Hygiene, Wonkwang Health Science University
Correspondence to Sung-Lim Lee, Department of Dental Hygiene, Wonkwang Health Science University, 514 Iksandae-ro, Iksan-si, Jeollabuk-do, 54538, Korea. Tel: +82-63-840-1321, Fax: +82-63-840-1269, E-mail: ymsllove@wu.ac.kr
Volume 24, Number 5, Pages 395-404, October 2024.
J Korean Soc Dent Hyg 2024;24(5):395-404. https://doi.org/10.13065/jksdh.20240504
Received on August 12, 2024 , Revised on August 24, 2024, Accepted on September 10, 2024, Published on October 30, 2024.
Copyright © 2024 Journal of Korean Society of Dental Hygiene.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License(http://creativecommons.org/licenses/by-nc/4.0)
Objectives: This study analyzed factors influencing oral health and quality of life in patients with dyslipidemia using raw data from the first year (2019) and third year (2021), where the quality of life was assessed using the HINT-8 tool from the 8th National Health and Nutrition Survey data. Methods: Frequency analysis, descriptive statistics, general linear model analysis, and linear regression analysis were performed on the collected data using SPSS program 26.0, and the data of 1,926 participants were analyzed. Results: The mean quality of life (HINT-8) score was 0.78 out of 1.00. Quality of life according to general characteristics, showed significant differences according to gender, age, household income, education level, lifetime smoking status, and lifetime alcohol consumption. In terms of oral health, it significantly differed according to chewing discomfort, speaking discomfort, oral examination history, toothbrushing frequency, toothache history, untreated dental care needs, subjective oral health status and use of oral care products. The predictors of quality of life were gender, household income, education level, lifetime alcohol consumption, chewing discomfort, speaking discomfort, toothache history, and untreated dental care needs. Conclusions: These results confirm that oral health influences the quality of life of patients with dyslipidemia and are expected to provide basic data for research on improving oral health and quality of life in these patients.
Dyslipidemia, Korea National Health and Nutrition Examination Survey, Oral health, Quality of life (HINT-8)
Cholesterol, an essential nutrient for the structure and maintenance of the human body, can be classified into three types: lowdensity lipoprotein cholesterol (LDL-C), known as ‘bad’ cholesterol and a major cause of atherosclerosis; triglycerides (TG), considered moderately harmful; and high-density lipoprotein cholesterol (HDL-C), known as ‘good’ cholesterol, which transports cholesterol from the blood and tissues to the liver for breakdown, helping prevent atherosclerosis [1].
Dyslipidemia refers to abnormal cholesterol levels in the blood, characterized by high levels of LDL-C, TG, or total cholesterol (LDL-C+HDL-C+TG), or low levels of HDL-C [2]. According to the Korean Society of Lipid and Atherosclerosis, dyslipidemia is diagnosed based on HDL-C <40 mg/dL, LDL-C ≥160 mg/dL, TG ≥200 mg/dL, or total cholesterol ≥240 mg/dL [3].
Cardiovascular disease (CVD) is one of the leading causes of death globally [4]. According to cause-of-death data from Statistics Korea (2022), heart disease (ranked 2nd), cerebrovascular disease (5th), and hypertensive diseases (9th) are among the top 10 causes of death in South Korea. The mortality rates for hypertensive diseases increased by 24.2%, cerebrovascular diseases by 12.6%, and heart diseases by 7.0% compared to the previous year [5]. Dyslipidemia is one of the four major risk factors for CVD in Koreans, alongside diabetes mellitus (DM), hypertension, and smoking [6]. Altered cholesterol levels lead to atherosclerosis, which in turn can cause or exacerbate CVD [7].
Data from the Health Insurance Review and Assessment Service shows that the number of patients with dyslipidemia increased by 38.4% from 2.19 million in 2019 to 3.04 million in 2023, marking a faster growth rate than that of hypertension (14.6%) and DM (19.2%) during the same period [8].
According to the 2022 Dyslipidemia Fact Sheet by the Korean Society of Lipid and Atherosclerosis, one in four adults aged 20 years or older has hypercholesterolemia, with its prevalence more than doubling between 2007 and 2020. Dyslipidemia affects 48.2% of all adults, with 72.1% of patients with hypertension and 87.1% of patients with DM also suffering from the condition. Although awareness and treatment rates for hypercholesterolemia are gradually increasing, three out of ten individuals remain unaware of their condition, and only about half are on lipid-lowering medications [3].
Risk factors for dyslipidemia include excessive intake of fats and carbohydrates, alcohol consumption, smoking, stress, obesity, lack of physical activity, aging, and menopause. Since the condition presents no noticeable symptoms, regular blood tests are essential for early detection and management to prevent complications such as angina, stroke, and myocardial infarction [7].
Interest in the link between dyslipidemia and oral health has been growing. Hwang [9] reported that individuals with fewer teeth were at greater risk of dyslipidemia and low HDL-C levels. Chen et al. [10] found that tooth loss was associated with lower cognitive scores and lower HDL-C levels. Choi [11] reported a higher prevalence of periodontitis in groups with abnormal levels of total cholesterol, HDL-C, LDL-C, and TG. Similarly, Griffiths and Barbour [12] found a correlation between high levels of LDL-C and TG and periodontal disease. Song et al. [13] suggested that frequent tooth brushing could improve lipid profiles, particularly HDL-C and TG, thereby reducing the risk of dyslipidemia.
Although previous studies have confirmed the relationship between dyslipidemia and oral health, particularly periodontitis, research that has explored the impact of dyslipidemia on oral health and quality of life using HINT-8 (Health-Related Quality of Life Instrument with 8 items) is scarce. This study aimed to analyze the factors affecting oral health and quality of life in patients with dyslipidemia, ultimately to provide valuable baseline data for future research on improving the oral health and quality of life in this population.
This study utilized the raw data from the first year (2019) (approval no. 2018-01-03-C-A) and the third year (2021) (approval no. 2018-01-03-3C-A) of the 8th Korea National Health and Nutrition Examination Survey (KNHANES) obtained using HINT-8. From a total sample of 15,200 individuals, 2,581 adults aged 20 and above who had been diagnosed with dyslipidemia were selected. After excluding cases with missing values for key variables, 1,926 dyslipidemia patients were included in the analysis <Fig. 1>.
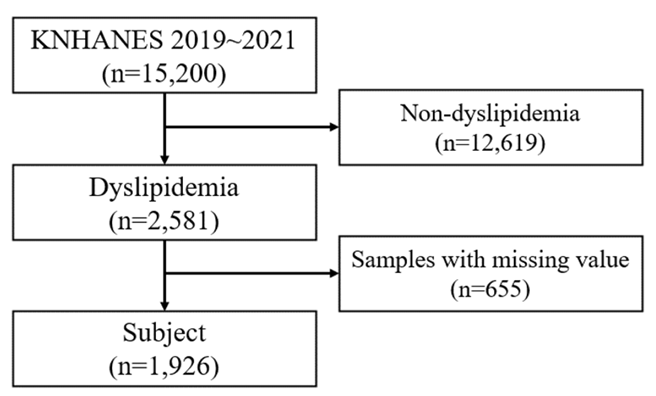
Fig. 1. Study participants
The HINT-8 tool used in this study was introduced in 2019 and has been used biennially. It assesses eight domains: climbing stairs, pain, energy, working, depression, memory, sleeping, and happiness, with responses categorized as ‘no problem,’ ‘little problem,’ ‘much problem,’ or ‘very much problem.’ A score closer to 1 indicates a higher quality of life. The characteristics that are evaluated include six items: gender, age, household income, education level, lifetime smoking status, and lifetime alcohol consumption. For oral health, chewing discomfort and speaking discomfort were reclassified as ‘discomfort’ if rated ‘significant discomfort’ or ‘discomfort,’ and ‘no discomfort’ if rated ‘neutral,’ ‘no discomfort,’ or ‘no discomfort at all.’ Toothbrushing frequency the previous day was categorized into three groups: ‘once or less,’ ‘twice,’ and ‘three times or more.’ Oral examination, toothache, and untreated dental care needs were categorized as ‘yes’ or ‘no.’ Subjective oral health status was categorized as ‘good’ if rated ‘very good’ or ‘good,’ and ‘not good’ if rated ‘average,’ ‘poor,’ or ‘very poor.’ The use of oral care products (floss, interdental brushes, mouthwash, electric toothbrushes, water flosser, tongue cleaners, implant brushes, and denture care products) was rated as ‘yes’ if any were used and ‘no’ otherwise.
In this study, we applied a complex sample analysis, with the stratified variable being the variance estimation strata (kstrata), the cluster variable being the primary sampling unit (psu), and combined weights from the health survey and health examination (wtitvex). Participants’ general characteristics, oral health, and quality of life were analyzed using descriptive statistics and frequency analysis. Differences in quality of life according to general characteristics and oral health were analyzed using analysis of variance (ANOVA) with a general linear model. Linear regression analysis was used to identify the predictors of quality of life. Statistical analysis was performed using the SPSS (ver. 26.0; IBM Corp., Armonk, NY, USA) software, and significance was set at 0.05.
Table 1 shows the HINT-8 results, including climbing stairs, pain, energy, working, depression, memory, sleeping, and happiness. The overall quality of life score was calculated based on the degree of problems reported for each item. The mean quality of life score was 0.78±0.00 out of 1.00.
Table 1. Participants’ quality of life
| Items | Division | N(%) |
|---|---|---|
| Climbing stairs | No | 759(43.5) |
| Little | 841(41.9) | |
| Much | 289(13.1) | |
| Very much | 37(1.5) | |
| Pain | No | 578(32.3) |
| Little | 1,024(52.7) | |
| Much | 271(12.8) | |
| Very much | 53(2.2) | |
| Energy | No | 581(29.9) |
| Little | 560(31.8) | |
| Much | 645(31.7) | |
| Very much | 140(6.6) | |
| Working | No | 819(44.7) |
| Little | 815(42.5) | |
| Much | 207(9.1) | |
| Very much | 85(3.7) | |
| Depression | No | 1,000(54.0) |
| Little | 789(39.4) | |
| Much | 101(5.2) | |
| Very much | 36(1.4) | |
| Memory | No | 683(38.4) |
| Little | 1,096(54.5) | |
| Much | 138(6.5) | |
| Very much | 9(0.5) | |
| Sleeping | No | 775(42.4) |
| Little | 863(43.6) | |
| Much | 261(12.8) | |
| Very much | 27(1.2) | |
| Happiness | No | 438(21.8) |
| Little | 566(31.7) | |
| Much | 766(39.1) | |
| Very much | 156(7.5) | |
| HINT-8 | 0.78±0.00* |
The data were analyzed by complex sample. *Mean±standard error (SE)
Quality of life in patients with dyslipidemia significantly differed according to gender (p<0.001), age (p<0.001), household income (p<0.001), education level (p<0.001), lifetime smoking status (p<0.001), and lifetime alcohol consumption (p<0.001). In terms of oral health, quality of life significantly differed according to chewing discomfort (p<0.001), speaking discomfort (p<0.001), oral examination history (p<0.001), toothbrushing frequency (p=0.002), toothache history (p<0.001), untreated dental care needs (p<0.001), subjective oral health status (p=0.011), and use of oral care products (p=0.008) <Table 2>.
Table 2. Quality of life (HINT-8) according to general and oral health
| Characteristics | Division | N(%) | Mean±SE | p* |
|---|---|---|---|---|
| Gender | Male | 709(43.2) | 0.81±0.00 | <0.001 |
| Female | 1,217(56.8) | 0.76±0.00 | ||
| Age (yr) | 20-39 | 54(4.2) | 0.82±0.01b | <0.001 |
| (Mean±SD: 61.06±0.37) | 40-64 | 929(57.5) | 0.80±0.00b | |
| ≥65 | 943(38.3) | 0.75±0.01a | ||
| Household income | Low | 548(23.2) | 0.73±0.01a | <0.001 |
| Mid-low | 538(27.4) | 0.77±0.01b | ||
| Mid-high | 423(23.9) | 0.80±0.01c | ||
| High | 417(25.5) | 0.82±0.01c | ||
| Education level | ≤Elementary school | 640(26.4) | 0.73±0.01a | <0.001 |
| Middle school | 323(14.8) | 0.78±0.01b | ||
| High school | 571(34.4) | 0.79±0.01b | ||
| ≥College | 392(24.4) | 0.82±0.01c | ||
| Lifetime smoking status | Yes | 710(42.5) | 0.80±0.01 | <0.001 |
| No | 1,216(57.5) | 0.77±0.00 | ||
| Lifetime alcohol consumption | Yes | 1,593(85.9) | 0.79±0.00 | <0.001 |
| No | 333(14.1) | 0.73±0.01 | ||
| Chewing discomfort | Yes | 565(27.2) | 0.73±0.01 | <0.001 |
| No | 1,361(72.8) | 0.80±0.00 | ||
| Speaking discomfort | Yes | 195(8.7) | 0.67±0.01 | <0.001 |
| No | 1,731(91.3) | 0.79±0.00 | ||
| Oral examination history | Yes | 770(42.4) | 0.80±0.00 | <0.001 |
| No | 1,156(57.6) | 0.77±0.00 | ||
| Toothbrushing frequency | ≤1 | 202(9.8) | 0.76±0.01a | 0.002 |
| 2 | 755(38.0) | 0.77±0.01a | ||
| ≥3 | 969(52.2) | 0.79±0.00b | ||
| Toothache history | Yes | 543(29.2) | 0.76±0.01 | <0.001 |
| No | 1,383(70.8) | 0.79±0.00 | ||
| Untreated dental care needs | Yes | 557(29.7) | 0.75±0.01 | <0.001 |
| No | 1,369(70.3) | 0.79±0.00 | ||
| Subjective oral health status | Good | 246(12.7) | 0.80±0.01 | 0.011 |
| Not good | 1,680(87.3) | 0.78±0.00 | ||
| Use of oral care products | Yes | 1,126(60.8) | 0.79±0.00 | 0.008 |
| No | 800(39.2) | 0.77±0.01 | ||
| Total | 1,926(100.0) |
*by complex sample general linear model
The predictors of quality of life in patients with dyslipidemia were identified as gender, household income, education level, lifetime alcohol consumption, chewing discomfort, speaking discomfort, toothache history, and untreated dental care needs (Table 3). Men had significantly higher quality of life than women (B=0.039, p<0.001), and higher household income was associated with significantly better quality of life compared to the lowest income group: mid-low (B=0.021, p=0.012), mid-high (B=0.029, p=0.003), and high (B=0.040, p<0.001). Similarly, higher education level were linked to better quality of life, with middle school graduates (B=0.024, p=0.004), high school graduates (B=0.023, p=0.003), and college graduates (B=0.033, p<0.001) showing significant improvements compared to those with less than an elementary school education. Lifetime alcohol consumption was also associated with significantly higher quality of life (B=0.025, p=0.010). In terms of oral health, those experiencing chewing discomfort had a significantly lower quality of life (B=-0.026, p<0.001), as did those with speaking discomfort (B=-0.069, p<0.001). Toothache history (B=-0.019, p=0.002) and untreated dental care needs (B=-0.028, p<0.001) were also associated with a significantly lower quality of life.
Table 3. Predictors of quality of life
| Characteristics | Division | B | SE | 95% CI | p* |
|---|---|---|---|---|---|
| Gender | Male | 0.039 | 0.008 | 0.024~0.054 | <0.001 |
| Female (ref.) | |||||
| Age (yr) | ≥65 | 0.001 | 0.012 | -0.023~0.026 | 0.930 |
| 40-64 | 0.003 | 0.013 | -0.022~0.029 | 0.784 | |
| 20-39 (ref.) | |||||
| Household income | High | 0.040 | 0.010 | 0.021~0.058 | <0.001 |
| Mid-high | 0.029 | 0.010 | 0.010~0.048 | 0.003 | |
| Mid-low | 0.021 | 0.008 | 0.005~0.038 | 0.012 | |
| Low (ref.) | |||||
| Education level | ≥College | 0.033 | 0.008 | 0.016~0.049 | <0.001 |
| High school | 0.023 | 0.008 | 0.008~0.038 | 0.003 | |
| Middle school | 0.024 | 0.008 | 0.008~0.039 | 0.004 | |
| ≤Elementary school (ref.) | |||||
| Lifetime smoking status | Yes | -0.009 | 0.008 | -0.025~0.007 | 0.278 |
| No (ref.) | |||||
| Lifetime alcohol consumption | Yes | 0.025 | 0.010 | 0.006~0.044 | 0.010 |
| No (ref.) | |||||
| Chewing discomfort | Yes | -0.026 | 0.007 | -0.040~-0.012 | <0.001 |
| No (ref.) | |||||
| Speaking discomfort | Yes | -0.069 | 0.013 | -0.094~-0.044 | <0.001 |
| No (ref.) | |||||
| Oral examination history | Yes | 0.002 | 0.006 | -0.009~0.013 | 0.710 |
| No (ref.) | |||||
| Toothbrushing frequency | ≥3 | 0.009 | 0.009 | -0.009~0.026 | 0.336 |
| 2 | 0.004 | 0.010 | -0.015~0.023 | 0.668 | |
| ≤1 (ref.) | |||||
| Toothache history | Yes | -0.019 | 0.006 | -0.032~-0.007 | 0.002 |
| No (ref.) | |||||
| Untreated dental care needs | Yes | -0.028 | 0.006 | -0.041~-0.016 | <0.001 |
| No (ref.) | |||||
| Subjective oral health status | Good | 0.006 | 0.007 | -0.008~0.021 | 0.406 |
| Not good (ref.) | |||||
| Use of oral care products | Yes | <0.001 | 0.006 | -0.013~0.013 | 0.976 |
| No (ref.) |
*by complex sample linear regression analysis
CI: Confidence interval; ref: reference
This study examined the factors affecting oral health and quality of life in patients with dyslipidemia using the HINT-8 data from the first (2019) and third (2021) years of the 8th KNHANES. Given the limited research in this area, the aim was to provide foundational insights for developing strategies to enhance the oral health and overall well-being of patients with dyslipidemia by analyzing the factors affecting their oral health and quality of life. To support the discussion, comparisons were made with data on the quality of life of patients with hypertension and DM, two other major chronic conditions prevalent in Korea.
The mean quality of life score for patients with dyslipidemia was 0.78 out of 1. This score was lower than the 0.92 reported for patients with hypertension using the EuroQol-5 dimension (EQ-5D) [14,15] and also lower than 0.87 [16] and 0.88 [17] reported for patients with DM using EQ-5D. This highlights the need for more comprehensive research encompassing the physical, mental, and social aspects to improve the quality of life of patients with dyslipidemia.
The predictors of quality of life in dyslipidemia patients included gender, household income, education level, lifetime alcohol consumption, chewing discomfort, speaking discomfort, toothache history, and untreated dental care needs. Men reported a significantly higher quality of life than women (B=0.039, p<0.001), which was consistent with the findings on patients with hypertension by Lee [14] and Han [18] and patients with DM by Kim and Cho [16]. The differences in quality of life between genders could be attributed to disparities in social and economic factors, such as fewer recreational and social activity involvement, lower education levels [19], higher proportion of oldest older adults, lower income, and poorer health status among women [20]. This underscores the need for targeted support for female patients with dyslipidemia to improve their quality of life.
Household income levels were significantly associated with quality of life, with those in the mid-low (B=0.021, p=0.012), mid-high (B=0.029, p=0.003), and high (B=0.040, p<0.001) brackets showing a significantly higher quality of life compared to the low-income group. Similarly, education level had a significant impact, with individuals who completed middle school (B=0.024, p=0.004), high school (B=0.023, p=0.003), and college or higher (B=0.033, p<0.001) reporting a higher quality of life than those with an elementary school education or less. These findings are consistent with previous studies on hypertension [14,21] and DM [22,23]. Higher household income and education level are critical factors for improving quality of life. Therefore, for patients with dyslipidemia who have lower income or education level, it is essential for the government and local communities to provide regular management, tailored education, and support to help improve their quality of life.
Lifetime alcohol consumption was associated with a higher quality of life (B=0.025, p=0.010), which aligns with research on hypertension [24,25] and DM [16,22]. Kim and Min [24] reported that alcohol consumption may help to alleviate stress and reduce depressive symptoms in the short term, but that further research is needed on this matter. Kim and Cho [16] posited that continuing alcohol consumption may temporarily address emotional issues, leading to a higher perceived quality of life in the short term. One of the causes of dyslipidemia is alcohol consumption, and excessive drinking can raise LDL cholesterol and triglyceride levels because alcohol itself contains calories, and it is often consumed with high-fat, high-calorie foods. More than half of patients with dyslipidemia are physically inactive, and 32% of women and 72% of men with the condition consume alcohol [3]. Hence, it is important to provide intervention programs promoting regular physical activity alongside alcohol cessation to improve the quality of life for patients with dyslipidemia.
The study also examined the impact of oral health on quality of life. Those experiencing discomfort while chewing had a significantly lower quality of life (B=-0.026, p<0.001), as did those with speaking discomfort (B=-0.069, p<0.001). Oral health is a critical factor for overall well-being, so poor oral health can lead to nutritional deficiencies, impaired chewing function, pain, and reduced productivity, all of which negatively impact both physical health and social interactions [26]. Periodontal disease has emerged as a leading cause of tooth loss and a major health problem that can impair quality of life, and the risk of dyslipidemia is higher with fewer existing teeth [9,10] and is associated with periodontitis and periodontal disease [11,12]. In this study, patients with dyslipidemia with chewing or speaking discomfort were found to have a lower quality of life. This finding aligns with studies on quality of life among patients with hypertension. Park and Yoon [27] also reported that patients with DM without chewing discomfort had a higher quality of life. Therefore, raising awareness among patients with dyslipidemia about the importance of addressing chewing and speaking discomfort through prevention and treatment could be critical to improving their quality of life.
Toothache history was another factor associated with lower quality of life (B=-0.019, p=0.002), consistent with findings from studies on hypertension [14] and adult populations by Jeong and Jang [28]. We could not compare these finding with those of patients with DM due to the limited research on this topic. The continuous management of dental caries and periodontal disease, which are the main causes of toothache, is crucial to improving the quality of life in patients with dyslipidemia.
Lee [29] found that having more untreated medical needs was associated with a lower overall quality of life, and Son [30] found that 9.0% of patients with hypertension experienced untreated medical needs that affected their quality of life. While there are no prior studies linking untreated dental care to quality of life, this study found that 29.7% of patients with dyslipidemia experienced untreated dental care, and those who did had significantly lower quality of life (B=-0.028, p<0.001). This highlights the need for comprehensive policies and expanded access to dental care services to improve both the oral health and quality of life of these patients.
This study faced limitations due to its cross-sectional design using the raw data from the first (2019) and third (2021) year of the 8th KNHANES and the lack of prior research on this specific population. Nonetheless, it provides valuable insights into the factors affecting oral health and quality of life in patients with dyslipidemia. Future research should build on these findings to develop comprehensive strategies aimed at improving the health outcomes and well-being of individuals with dyslipidemia.
In this study, the relationship between oral health and quality of life in patients with dyslipidemia was analyzed using raw data obtained with the HINT-8 from the first (2019) and third year (2021) of the 8th KNHANES. The following results were obtained from an analysis of 1,926 participants:
1. The mean quality of life (HINT-8) score was 0.78 out of 1.00.
2. Quality of life according to general characteristics, showed significant differences according to gender (p<0.001), age (p<0.001), household income (p<0.001), education level (p<0.001), lifetime smoking status (p<0.001), and lifetime alcohol consumption (p<0.001). In terms of oral health, it significantly differed according to chewing discomfort (p<0.001), speaking discomfort (p<0.001), oral examination history (p<0.001), toothbrushing frequency (p=0.002), toothache history (p<0.001), untreated dental care needs (p<0.001), subjective oral health status (p=0.011), and use of oral care products (p=0.008).
3. The predictors of quality of life were gender, household income, education level, lifetime alcohol consumption, chewing discomfort (B=-0.026, p<0.001), speaking discomfort (B=-0.069, p<0.001), toothache history (B=-0.019, p=0.002), and untreated dental care needs (B=-0.028, p<0.001).
These results demonstrate that oral health impacts the quality of life of patients with dyslipidemia. We hope that these findings serve as valuable foundational data for future research promoting oral health and quality of life in this population.
The author fully participated in the work performed and documented truthfully.
The author declared no conflicts of interest.
This paper was supported by Wonkwang Health Science University in 2024.
None.
Data can be obtained from the corresponding author.
None.
1. The Korean Society of Lipid and Atherosclerosis. Cholesterol [Internet][cited 2024 Jul 30]. Available from: https://www.lipid.or.kr/dyslipidemia_arteriosclerosis/lipids.php.
2. Korea Disease Control and Prevention Agency. Dyslipidemia prevention and management information for me and my family 2023 [Internet][cited 2024 Jul 30]. Available from: https://health.kdca.go.kr/healthinfo/biz/health/ntcnInfo/helthEdcRecsroom/helthEdcRecsroomView.do?phledu_recsroom_sn=1703.
3. The Korean Society of Lipid and Atherosclerosis. Dyslipidemia fact sheet in Korea. 2022. Seoul: The Korean society of lipid and atherosclerosis; 2022: 1-52.
4. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, April P, et al. Heart disease and stroke statistics-2019 update: a report From the American Heart Association. Crculation 2019;139(10):e56-e528. https://doi.org/10.1161/CIR.0000000000000659
[DOI][PubMed]
5. Statistics Korea. Cause of death statistics for 2022 [Internet][cited 2024 Aug 01]. Available from: https://www.kostat.go.kr/board.es?mid=a10301010000&bid=218&act=view&list_no=427216.
6. Lee KJ. Relationship between relative handgrip strength and dyslipidemia in non-patient[Master’s thesis]. Seoul: Yonsei University, 2022.
7. Korea Disease Control and Prevention Agency. Dyslipidemia [Internet][cited 2024 Aug 01]. Available from: https://health.kdca.go.kr/healthinfo/biz/health/gnrlzHealthInfo/gnrlzHealthInfo/gnrlzHealthInfoView.do.
8. The JoongAng. Dyslipidemia, the most fatal disease in the world, and the number of teenage patients is also on the rise [Internet][cited 2024 Aug 01]. Available from: https://www.joongang.co.kr/article/25264760#home
9. Hwang DG. Relationship of dyslipidemia and oral chewing status in the elderly[Master’s thesis]. Daegu: Kyungpook National University, 2024.
10. Chen HM, Li KY, Li TL, Kwong E, Yan Wong GH, McGrath C, et al. The association between tooth loss and cognitive decline in the aged population: the mediating role of HDL-cholesterol. J Dent 2023;135:104570. https://doi.org/10.1016/j.jdent.2023.104570
[DOI][PubMed]
11. Choi JS. Association between periodontitis and hypertriglyceridemia in Korean adults aged 30 and older: based on data from 2015 Korea National Health and Nutrition Examination Survey. J Korean Soc Dent Hyg 2020;20(1):53-62. https://doi.org/10.13065/jksdh.20200006
[DOI]
12. Griffiths R, Barbour S. Lipoproteins and lipoprotein metabolism in periodontal disease. Clin Lipidol 2010;5(3):397-411. https://doi.org/10.2217/clp.10.27
[DOI][PubMed][PMC]
13. Song TJ, Kim JW, Kim JW. Oral health and changes in lipid profile: a nationwide cohort study. J Clin Periodontol 2020;47(12):1437-45. https://doi.org/10.1111/jcpe.13373
[DOI][PubMed]
14. Lee SL. A study on oral health and quality of life in patients with hypertension. J Korean Soc Dent Hyg 2023;23(5):361-8. https://doi.org/10.13065/jksdh.20230040
[DOI]
15. Im JY. Relevant factors and levels of the quality of life among in aged 40 and over with hypertension patients[Master’s thesis]. Daejeon: Chungnam National University, 2020.
16. Kim SH, Cho SH. Factors influencing the quality of life (EQ-5D) of patients with diabetes mellitus: study based on data from the second annual Korea health panel survey (2019). KSIM 2023;11(3):99-114. https://doi.org/10.15268/ksim.2023.11.3.099
[DOI]
17. Jee YJ, Park YS. Factors influencing the quality of life of diabetics. AJMAHS 2019;9(10):459-67. https://doi.org/10.35873/ajmahs.2019.9.10.039
[DOI]
18. Han MH. Health behavior, disease management, and factors related quality of life of young adults with hypertension or diabetes: 2019 Community Health Survey. Korean Public Health Research 2022;48(3):1-17. https://doi.org/10.22900/kphr.2022.48.3.001
[DOI]
19. Castellano-Guerrero AM, Guerrero R, Ruiz-Aranda D, Perea S, Pumar A, Relimpio F, et al. Gender differences in quality of life in adults with long-standing type 1 diabetes mellitus. Diabetol Metab Syndr 2020;17(12):64. https://doi.org/10.1186/s13098-020-00571-x
[DOI][PubMed][PMC]
20. Orfila F, Ferrer M, Lamarca R, Tebe C, Domingo-Salvany A, Alonso J. Gender differences in health-related quality of life among the elderly: the role of objective functional capacity and chronic conditions. Soc Sci Med 2006;63(9):2367-80. https://doi.org/10.1016/j.socscimed.2006.06.017
[DOI][PubMed]
21. Kim SI, Woo SJ, Jung YH. Factors related to hypertension patients’ quality of life: the 7th Korean National Health and Nutrition Examination(1st year, 2016). JKSSCHE 2020;21(1):61-74. https://doi.org/10.35133/kssche.20200531.05
[DOI]
22. Lim JH, Oh CS. Medical care utilization status and quality of life in diabetes mellitus patients. The Journal of Digital Policy & Management 2013;11(10):609-18.
23. Lee EK, Jung SY. Associated factors with health-related quality of life among older adults with diabetes in Korea. Korean J Rehabil Nurs 2022;25(2):61-9. https://doi.org/10.7587/kjrehn.2022.61
[DOI]
24. Kim HJ, Min ES. Health behaviors and quality of life by life cycle of hypertensive patients. J Converg Inf Technol 2020;10(7):58-66. https://doi.org/10.22156/CS4SMB.2020.10.07.058
[DOI]
25. Lee KE, Cho EH. Factors influencing health related quality of life in patients with hypertension: based on the 5th Korean National Health and Nutrition Examination Survey. Jour. of KoCon.a 2016;16(5):399-409. https://doi.org/10.5392/JKCA.2016.16.05.399
[DOI]
26. Reisine ST. Dental disease and work loss. J Dent Res 1982;61(10):1158-62. https://doi.org/10.1177/00220345820610100901
[DOI][PubMed]
27. Park CM, Yoon HS. Oral management behavior and EQ-5D index of older adults over 65 years of age diagnosed with diabetes. JNCIST 2022;6(11):2214-22. https://doi.org/10.33097/JNCTA.2022.06.11.2214
[DOI]
28. Jeong SR, Jang JE. The effects of toothache experience and oral health behavior on health-related quality of life in Korean adultsusing the second edition of the 8th National Health Nutrition Survey (2019-2020). J Korean Acad Oral Health 2022;46(4):169-73. https://doi.org/10.11149/jkaoh.2022.46.4.169
[DOI]
29. Lee JW. Effect of unmet healthcare needs on quality of life. JKAIS 2020;21(9):283-90. https://doi.org/10.5762/KAIS.2020.21.9.283
[DOI]
30. Son MS. Factors associated with unmet healthcare needs in adults with hypertension: based on the eighth Korea National Health and Nutrition Examination Survey 2019. J Korean Assn Learn Cent Curric Instr 2022;22(19):149-58. https://doi.org/10.22251/jlcci.2022.22.19.149
[DOI]