1Department of Dental Hygiene, Ulsan College
2Department of Dental Hygiene, Masan University
3Department of Dental Hygiene, Dong-eui University
4Oral Hygiene Science Research Institute, Dong-eui University
Correspondence to Jung-Hwa Lee, Department of Dental Hygiene, Dong-eui University, 176 Eomgwang-ro, Busanjin-gu, Busan-si, 47340, Korea. Tel: +82-51-890-4239, Fax: +82-505-182-6878, E-mail: yamako93@deu.ac.kr
Volume 24, Number 4, Pages 291-300, August 2024.
J Korean Soc Dent Hyg 2024;24(4):291-300. https://doi.org/10.13065/jksdh.20240403
Received on June 07, 2024 , Revised on July 10, 2024, Accepted on July 10, 2024, Published on August 30, 2024.
Copyright © 2024 Journal of Korean Society of Dental Hygiene.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License(http://creativecommons.org/licenses/by-nc/4.0)
Objectives: To develop a program that combines the oral health promotion program for the elderly and to investigate the effect of improving oral function by applying the oral health promotion program to elderly people using welfare facilities. Methods: From June to October 2022, a total of 29 elderly individuals utilizing welfare facilities in the Gyeongnam region were recruited. The control group underwent surveys and objective oral health assessments. The experimental group participated in an oral health promotion program, consisting of oral functional rehabilitation exercises and expert oral health management, conducted once a week for 8 weeks at the facilities. Objective oral health assessments were conducted before, during (at 4 weeks), and after (at 8 weeks) the intervention period for both groups. Results: As a result of the oral health promotion program, it was confirmed that there was an improvement effect in bad breath (p<0.001), saliva secretion amount (p<0.001), orbicularis oculi muscle (p<0.001), and plaque index (p<0.001). Conclusions: A revitalization plan is needed so that the efficient oral health promotion program for the elderly can be reflected as a systematic and professional community care oral health management program.
Elderly, Oral function rehabilitation exercises, Oral health promotion, Professional oral health care
According to data from the Health Insurance Review & Assessment Service, healthcare expenditures for older adults covered by health insurance increased by more than 1.5-fold between 2010 and 2015, from 14.135 to 21.921 billion KRW, placing a significant burden on the social security system [1]. In response to this increase, the Ministry of Health and Welfare established a task force in 2018 to build an integrated care service for vulnerable populations, as part of a comprehensive approach addressing the complex issues of an aging society. By 2020, they launched a pilot program–the Korean community care initiative–in 16 local governments, with Cheonan and Bucheon conducting home oral health interventions [2].
The oral cavity is an essential component of energy intake via mastication and plays a crucial role in overall health. Poor oral health can lead to systemic health deterioration, nutritional imbalances, and reduced quality of life, making oral health increasingly important as people age [3]. Among older adults, oral infections caused by apical and periodontal lesions, poor dentures, or restorations can escalate into life-threatening systemic infections [4] or increase the risk of cardiovascular disease, stroke, diabetes mellitus, and respiratory disease due to the spread of bacteria through the bloodstream [5].
Additionally, medications for systemic diseases often cause xerostomia in older adults, with 48.1% of individuals >65 years of age experiencing oral discomfort [6,7]. Xerostomia affects mastication, swallowing, pronunciation, and taste and can result in a burning sensation, leading to nutritional imbalances. A dry oral environment and poor oral hygiene can facilitate respiratory pathogen colonization in the oropharynx, increasing the risk of aspiration pneumonia, which has a mortality rate four times higher than that of general pneumonia in older adults [8,9].
Numerous studies have been conducted on oral health in the Korean population. Moon [10] reported improvements in halitosis and plaque index through a toothbrushing program. Choi [11] highlighted the effects of professional oral care, including toothbrushing and denture disinfection, on salivary secretion, halitosis, and bacterial count in long-term care hospital patients. Lee [12] demonstrated improvements in plaque, halitosis, tongue coating, and salivary secretion through professional oral care, including toothbrushing, scaling, denture cleaning, oral muscle and salivary gland massage, and tongue-cheek articulation exercises. Lee et al. [13] reported the benefits of oral exercises for residents of long-term care facilities, including increased repetition of swallowing and pronunciation, salivary volume, mouth opening, and cheek puffing. Kim and Lee [14] also observed improvements in muscle function through oral and tongue strengthening exercises.
Jang and Lee [15] documented the impact of a program promoting oral health which combined oral exercises and the Watanabe tooth-pick method of toothbrushing on pronunciation, swallowing, and salivary secretion in older adults. Moon [10] showed enhancements in plaque and gingival bleeding indices, halitosis, and oral moisture by providing toothbrushing videos and posting posters about facial muscle, tongue, and salivary gland stimulation exercises in long-term care units to encourage residents to practice these activities three times daily. Studies integrating both oral function exercises and professional oral care, however, remain limited.
Based on findings that party blowers promote the activation of nerves and muscles related to nasopharyngeal closure [16], in addition to being easy to obtain and entertaining, we chose party blowers as our instrument for this study. Additionally, the findings of Lee et al. [17] that gum chewing is effective for alleviating xerostomia, we opted to utilize gum chewing as well, to improve salivary secretion and buffering capacity in older adults.
This study aimed to provide foundational data on the oral health status and functional improvement of older adults through an 8-week program combining oral-motor exercises (tongue and orbicularis oris strength, salivary gland stimulation) and professional oral care (sponge brush, Watanabe method, modified bass method, dental floss, interdental brushing, gum massage). Our overall goal was to validate the effectiveness of oral health programs provided by care facilities and public organizations.
This study, conducted from June 2022 to October 2022, was approved by the Institutional Review Board of Dong-eui University (IRB No. DIRB-202205-HR-E-12) for the ethical protection of human subjects.
Older adults aged 65 years or older residing at the D Senior Welfare Center in Busan, Ulsan, and Yangsan E Senior Welfare Center in Gyeongsangnam-do who voluntarily provided informed consent to participate in the study were enrolled. After excluding edentulous individuals, those wearing complete dentures, and those diagnosed with coronavirus disease 2019 (COVID-19) during the program, the sample size was calculated using a sampling program (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany Power 3.19). For a moderate effect size of F=0.40, power=0.80, and significance level of α=0.05, the minimum sample size was calculated to be 28. In consideration of a potential dropout rate of 30%, 36 patients were enrolled. After excluding 7 participants who did not complete the questionnaire and poorly attended the program sessions, 29 participants were included in the final analysis.
Each patient’s general, health-related, and oral health-related characteristics were surveyed before the program. The control group was managed without intervention, while the experimental group received guidance on oral function exercises and professional oral health care.
The control group received objective oral health examinations (halitosis, salivation, dental plaque index, orbicularis oris muscle strength) and questionnaires before the oral health initiative started, week 4 and week 8, while the experimental group received guidance on oral function exercises and professional oral health care. Oral function exercises consisted of daily use of a party blower and gum chewing. Oral healthcare professionals visited the facility once a week for 8 weeks to provide sponge, Watanabe method, modified bass method, and interdental brushing, as well as flossing and gum massage. The experimental group underwent objective oral health examinations before starting the oral health program, weeks 4 and 8 of the program. The study flowchart is shown in <Fig. 1>.
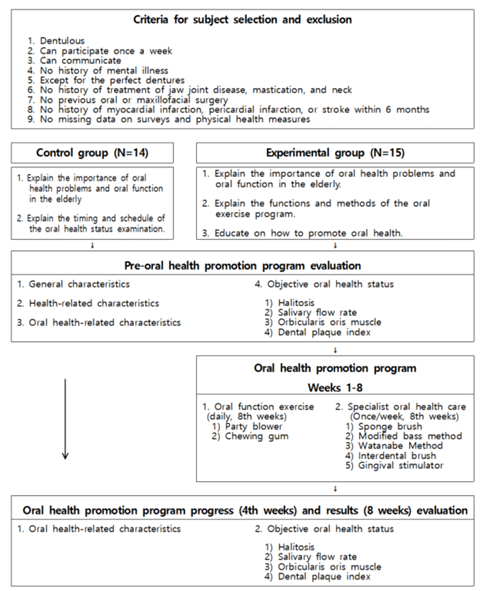
Fig. 1. Research process
In this study, we assessed the objective oral health status after patients underwent a program which included professional oral care and oral function rehabilitation exercises. To minimize errors, both the researcher and research assistants were provided with detailed manuals and training on the measurement methods used before and after the program.
Participants were instructed to perform daily oral function exercises, including gum chewing and using a party blower. They were asked to place a sticker in a research diary (calendar) after each exercise session to track their adherence, which the researcher evaluated weekly to ensure compliance. Professional oral care was provided once a week for 8 weeks. The researcher and two assistants visited the senior residential centers weekly, from 9:00 AM to 11:30 AM, to provide oral care in the following order: sponge, Watanabe method, and modified bass method brushing, flossing, interdental brushing, and gum massage.
(1) Party blower
The party blower used in this study refers to a device that forms the shape of an elephant’s trunk when blown. The blower (9 cm internal diameter) is made of polyvinyl chloride (PVC) and is connected to a tube that measures 6 cm in length×1 cm in thickness. Participants were instructed to blow the party blower for 10 seconds, four times per set. Two sets were performed in the morning and again in the evening. Participants were advised to rest sufficiently after each set to avoid respiratory muscle fatigue. They were also instructed to stop the exercise if they experienced breathing difficulties or dizziness, and to record the details in a sticker calendar.
(2) Gum chewing
Participants were instructed to chew a small piece of commercially available gum containing at least 67% xylitol for 20 minutes. For gum chewing, the subjects chewed commercially available gum containing more than 67% xylitol twice a day for 20 minutes and then spit it out.
During the objective oral health examinations, we evaluated halitosis, salivation, orbicularis oris muscle strength, and dental plaque indices.
(1) Halitosis
Halitosis was measured using a handheld halitosis meter (HC-212S-WH; Tanita, Tokyo, Japan) as described by Joung [18]. The degree of halitosis was measured in six levels, ranging from 0 for no halitosis to 5 for very severe halitosis.
(2) Salivation
Salivary secretions were measured by having participants chew paraffin wax (Saliva-Check BUFFER; GC, Tokyo, Japan ) for 5 minutes. The stimulated saliva was collected in a graduated test tube and the volume was recorded(ml).
(3) Orbicularis oris muscle strength
Orbicularis oris muscle strength was measured using an Oral Immunization Training Appliance (Litre Meter, Oral Academy, Tokyo, Japan) with a soft mouthpiece. Participants gently bit the mouthpiece with their upper and lower teeth, positioned it between their lips and teeth, and then pulled the Litre Meter device horizontally until the mouthpiece seemed about to slip out from their lips. At this point, the pulling force was recorded. Normal values for adults are around 2.0 kg, while for older adults, they are ≥1.4 kg. Scoring was based on the following guidelines: 1 point for <1.0 kg, 2 points for 1.0–1.49 kg, and 3 points for ≥1.5 kg [19].
(4) Dental plaque
Dental plaque was assessed using a modified Patient Hygiene Performance Index by Podshadley and Haley [20]. Six teeth (#16, 26, 36, 46, 11, 31) were covered with a solution and lightly brushed. The adherence of the dental plaque above the gingival margin was then measured. Each tooth was scored as follows: 0 for no staining, 1 for staining in one area, and 5 for staining of the entire tooth.
The collected data were statistically analyzed using SPSS program (ver. 25.0; IBM Corp., Armonk, NY, USA), with a significance level set at p<0.05. The normality of the oral health data was evaluated using the Shapiro-Wilk test. Results indicated that orbicularis oris muscle strength and salivary secretion volumes were normally distributed, allowing for parametric homogeneity tests. For nonnormally distributed data, non-parametric methods were used for homogeneity testing. General characteristics and homogeneity of oral health status characteristics were analyzed using the Chi-squared test. The baseline homogeneity of oral health status (halitosis, salivary secretion volume, dental plaque index, orbicularis oris muscle strength) was assessed using independent sample t- and non-parametric Mann-Whitney U tests. Differences in oral health status before the program, at 4 weeks, and at 8 weeks were analyzed using repeated measures analysis of variance (ANOVA).
In terms of general characteristics, the control and experimental groups were found to be homogeneous, with no significant differences between the two groups among all variables (p>0.05) <Table 1>.
Table 1. Homogeneity test according to general characteristics
Unit: N(%)
| Characteristics | Division | Control group (N=14) | Experimental group (N=15) | Total (N=29) | χ² | p* |
|---|---|---|---|---|---|---|
| Sex | Man | 7(50.0) | 3(20.0) | 10(34.5) | 2.885 | 0.095 |
| Woman | 7(50.0) | 12(80.0) | 19(65.5) | |||
| Age (yr) | ≤65 | 3(21.4) | 2(13.3) | 5(17.2) | 0.546 | 0.884 |
| 66-75 | 7(50.5) | 9(60.0) | 16(55.2) | |||
| ≥76 | 4(28.6) | 4(26.7) | 8(27.6) | |||
| Education | Elementary | 1(7.1) | 4(26.7) | 5(17.2) | 2.906 | 0.236 |
| Middle school | 5(35.7) | 2(13.3) | 7(24.1) | |||
| ≥High school | 8(57.1) | 9(60.0) | 17(58.6) | |||
| Smoking | No | 3(21.4) | 2(13.3) | 5(17.2) | 0.333 | 0.651 |
| Yes | 11(78.6) | 13(86.7) | 24(82.8) | |||
| Presence of systemic disease | No | 3(21.4) | 5(33.3) | 8(27.6) | 0.514 | 0.682 |
| Yes | 11(78.6) | 10(66.7) | 21(72.4) |
*by chi-square test
There were no significant differences in halitosis, salivation, dental plaque index, and orbicularis oris muscle strength between the two groups, confirming homogeneity (p>0.05) <Table 2>.
Table 2. Homogeneity test of dependent variable
Unit: Mean±SD
| Variable | Division | Control group (N=14) | Experimental group (N=15) | t/Z | p* |
|---|---|---|---|---|---|
| Objective oral health status | Bad breath† | 2.21±0.70 | 2.47±0.74 | 0.837 | 0.451 |
| Salivary flow rate | 6.00±1.66 | 6.33±2.09 | -0.472 | 0.640 | |
| Dental plaque index† | 25.79±27.25 | 27.69±16.67 | 1.026 | 0.310 | |
| Orbicularis oris muscle | 0.90±0.38 | 0.64±0.36 | 1.886 | 0.070 |
*by t-t est,†by Mann- Whitney U test
ANOVA was used to analyze the effects of the oral health promotion program on oral function and health status between the control and experimental groups before and after the intervention. The results indicated that halitosis significantly decreased in the experimental group, by 1.95 points, from 2.47 before the intervention to 1.20 at 4 weeks and 0.53 at 8 weeks (p<0.001). The group and time interaction effect was significant (p<0.001). Salivary secretion volumes in the experimental group increased significantly, by 0.93 points, from 6.33 before the intervention to 7.10 at 4 weeks and 7.27 at 8 weeks (p<0.001). However, the group and time interaction effect was not significant. The dental plaque indices in the experimental group decreased significantly, by 15.06 points, from 27.69 before the intervention to 16.19 at 4 weeks and 12.63 at 8 weeks (p<0.001). The group and time interaction effect was significant (p<0.01). Orbicularis oris muscle strength in the experimental group significantly increased, by 0.93 points, from 0.64 before the intervention to 1.13 at 4 weeks and 1.57 at 8 weeks (p<0.001). The group and time interaction effect was also significant (p<0.001) <Table 3>.
Table 3. Test for differences in changes in bad breath, saliva flow rate, dental plaque index, and orbicularis oris muscle at each time point
Unit: Mean±SD
| Variables | Control group (N=14) | Experimental group (N=15) | F(p*) (Group) |
F(p*) (Time × group) |
||||
|---|---|---|---|---|---|---|---|---|
| Program pre-inspection | Program under inspection (4th weeks) | Program after inspection (8th weeks) | Program pre-inspection | Program under inspection (4th weeks) | Program after inspection (8th weeks) | |||
| Bad breath | 2.21±0.70 | 2.21±0.70 md=0.00, p=1.000 |
2.21±0.70 md=0.00, p=1.000 md=0.00, p=1.000 |
2.47±0.74 | 1.20±1.57 md=-1.27, p<0.001 |
0.53±1.30 md=-0.67, p=0.003 md=-1.93, p<0.001 |
118.723 (<0.001) |
18.487 (<0.001) |
| Saliva flow rate | 6.00±1.66 | 6.07±1.44 md=0.07, p=0.880 |
6.21±1.48 md=0.14, p=0.761 md=0.21, p=0.679 |
6.33±2.09 | 7.10±2.74 md=0.77, p=0.103 |
7.27±2.58 md=0.17, p=0.713 md=0.93, p=0.070 |
377.228 (<0.001) |
0.741 (0.482) |
| Dental plaque index | 25.79±27.25 | 26.32±26.09 md=0.53, p=0.851 |
24.79±20.60 md=-1.54, p=0.581 md=-1.01, p=0.781 |
27.69±16.67 | 16.19±11.83 md=-11.49, p<0.001 |
12.63±12.68 md=-3.57, p=0.190 md=-15.06, p<0.001 |
40.596 (<0.001) |
6.353 (0.003) |
| Orbicularis oris muscle | 0.90±0.38 | 0.91±0.38 md=0.01, p=0.912 |
0.91±0.39 md=0.01, p=0.895 md=0.01, p=0.854 |
0.64±0.36 | 1.13±0.27 md=0.49, p<0.001 |
1.57±0.33 md=0.44, p<0.001 md=0.93, p<0.001 |
280.241 (<0.001) |
50.294 (<0.001) |
md: mean difference, *by repeated measures ANOVA
Comparison between time points was performed using paired t-test.
This study aimed to develop an oral health promotion program consisting of professional oral care and oral function rehabilitation exercises for older adults, and to assess the effects of this program over an 8-week period as compared to a control group.
Repeated measures ANOVA showed a significant reduction in halitosis between the control and experimental groups after the 8-week oral health promotion program. Although Moon [10] did not find significant differences between the experimental and control groups, their results showed significant group and time interaction effects, in line with our findings. Moon [10], Lee [12], Park and Sohng [20], and Munro [21] all demonstrated the effectiveness of professional oral care in reducing halitosis and dental plaque indices, also in line with the results of this study.
Repeated measures ANOVA revealed significant differences in salivary secretion volumes between the two groups after the 8-week program, but no significant interaction effects between time points and groups. This suggests that while the experimental group showed an increase in salivary secretion, it was not significantly different than the control group. Studies by Jeon et al. [22] and Jang et al. [23] support these findings, indicating the need for continuous oral function improvement exercises to maintain increased salivary secretion, which helps reduce halitosis and improves swallowing, pronunciation, and tongue movement.
Repeated measures ANOVA showed significant differences in dental plaque indices after the 8-week program, as well as significant interaction effects between time points and groups. These findings are consistent with the study by Moon [10], which demonstrated the effectiveness of professional oral care, including the Watanabe toothbrushing method and interdental brushes, in managing dental plaque.
Repeated measures ANOVA indicated significant differences in orbicularis oris muscle strength after the 8-week program, as well as significant interaction effects between time points and groups. Studies by Kim and Lee [14] and Jang and Lee [15] reported improvements in swallowing disorders, swallowing power, and tongue pressure in older adults through combined oral exercises, which support our findings. This suggests that oral function rehabilitation exercises positively impact orbicularis oris muscle strength.
This study had a few limitations. Due to the COVID-19 pandemic, the program duration was limited to 8 weeks, and given that the study was conducted only in the Busan, Ulsan, and Gyeongnam areas, the findings have limited generalizability. Future studies should expand the program’s implementation across different regions and extend the duration to at least 6 months to more thoroughly evaluate its effectiveness and validity as part of oral health policies for older adults.
This study aimed to verify the effects of professional oral care and oral function rehabilitation exercises on the oral health status of older adults. The study included two groups: a control group of 14 participants and an experimental group of 15 participants. The experimental group received professional oral care and oral function rehabilitation exercises while the control group underwent evaluations and completed questionnaires. The key findings were as follows:
1. Halitosis significantly decreased, by 1.93 points, from 2.47 before the intervention to 0.53 after 8 weeks (p<0.001), with significant interaction effects over time (p<0.001).
2. Salivary secretion volumes increased by 0.93, from 6.33 before the intervention to 7.27 after 8 weeks (p<0.001). However, there were no significant interaction effects over time.
3. The dental plaque indices decreased significantly, by 15.06 points, from 27.69 before the intervention to 12.63 after 8 weeks (p<0.001), with significant interaction effects over time (p<0.01).
4. Orbicularis oris muscle strength increased by 0.93, from 0.64 before the intervention to 1.57 after 8 weeks (p<0.001), with significant interaction effects over time (p<0.001).
The results of this study indicate that professional oral care and oral function rehabilitation exercises significantly improved the objective oral health status (halitosis, salivary secretion volumes, dental plaque indices, orbicularis oris muscle strength) of older adults aged ≥ 65. Therefore, applying the professional oral care and oral function rehabilitation exercise program used in this study in clinical and community settings could enhance both oral and overall health, in older adults. Accordingly, it is important to develop and integrate a systematic and professional community care oral health management program based on the professional oral care and oral function rehabilitation exercises utilized in this study.
Conceptualization: AJ Jeong, NS Kim, JH Lee; Data collection: AJ Jeong; Formal analysis: AJ Jeong; Writing-original draft: AJ Jeong, JH Lee; Writing-review and editing: AJ Jeong, NS Kim, JH Lee
The authors declared no conflicts of interest.
None.
The institutional review board of Dong-eui University (No. DIRB-202205-HR-E-12) approved the study, ensuring ethical protection for the participants.
Data can be obtained from the corresponding author upon reasonable request.
This paper was an excerpt from Ae-Jin Jeong thesis for doctoral dissertation in 2022.
This manuscript is a revision of the first author’s Doctoral dissertation from Dong-eui University.
1. Health insurance review and assessment service Korea. Trends and factors of increase in health insurance elderly care expenses from 2010 to 2015 [Internet]. Health insurance review and assessment service Korea policy trends.[cited 2022 Jan 02]. Available from: https://repository.hira.or.kr/bitstream/2019.oak/1096/2/2010-2015년%20건강보험%20노인진료비의%20추이%20및%20증가요인.pdf.
2. Jang JH, Cho JW, Kim YJ, Ki JY, Jo KS, Kim JR, et al. Preliminary study for the development of a visiting oral health care intervention program for the elderly based on community healthcare. J Korean Acad Oral Health 2020;44(3):166-72. https://doi.org/10.11149/jkaoh.2020.44.3.166
[DOI]
3. Kim YG. Geriatric dental hygiene care. Seoul: Komoonsa; 2020: 46-253.
4. Yasny J, Silvay G. Geriatric patients: oral health and the operating room. J Am Geriatr Soc 2010;58(7):1382-5. https://doi.org/10.1111/j.15325415.2010.02919.x
[DOI][PubMed]
5. Yun JH, Lim KO, Relationship between the number of remaining teeth and multimorbidity in Korea older adults (KNHANES 2014-2018). J Next-generation Convergence Technology Association 2022;6(3):445-52. https://doi.org/10.33097/JNCTA.2022.06.03.445
[DOI]
6. Jo SR, Cho JW, Jang JH. Effect of probiotics intake on oral environment changes of the elderly in long-term care facilities. J Korean Soc Dent Hyg 2020;20(5):753-62. https://doi.org/10.13065/jksdh.20200069
[DOI]
7. Korea Institute for Health and Social Affairs. 2014 Survey on public health nutrition [Internet]. Sejong: Ministry of Health & Welfare; 2022.[cited 2021 May 05]. Available from: https://knhanes.cdc.go.kr/knhanes/index.do.
8. Kim JH, Kim HY. Effects of an oral self-care program on the elderly’s xerostomia and oral health-related quality of life. J Korean Acad Community Health Nurs 2018;29(3):382-92. https://doi.org/10.12799/jkachn.2018.29.3.382
[DOI]
9. Rhyou KS, Yang YH. Characteristics and clinical outcomes of elders with aspiration pneumonia. J Korean Gerontol Nurs 2018;20(1):45-55. https://doi.org/10.17079/jkgn.2018.20.1.45
[DOI]
10. Moon SH. Effect of integrated oral health care program for older adults in long-term care facilities [Doctoral dissertation]. Seoul: Hanyang University, 2018.
11. Choi SM. The effects of professional oral health care on oral health states of long-term care patients in geriatric hospital [Doctoral dissertation]. Daegu: Yeungnam University, 2011.
12. Lee GY. Development and evaluation of professional oral care program for elderly in long-term care facilities [Doctoral dissertation]. Seoul: Seoul National University, 2017.
13. Lee JH, Kwon HK, Lee YH, Lee MH, Lee HK. Effect of regular oral exercise on oral function in elderly patients with long-term care. J Korean Acad Oral Health 2010;34(3):422-9.
14. Kim NS, Lee JH. Effects of tongue strength training program combined with oral exercises on swallowing disorder swallowing ability and tongue pressure in the elderly. J Korean Soc Dent Hyg 2023;23(2):105-13. https://doi.org/10.13065/jksdh.20230011
[DOI]
15. Jang JY, Lee DH. Effects of oral health promotion program on oral function in the elderly. Korean J Health Ser Manag 2016;10(4):141-51. https://doi.org/10.12811/kshsm.2016.10.4.141
[DOI]
16. Kwon HS, Kim CS, Oh SH, Lee MO, Lee SM, Lee JH, et al. Oral rehabilitaion. 4th ed. Seoul: Jisung; 2018: 85-6.
17. Lee EK, Jun HJ, Kim MJ, Park JW, Ko SJ. A review of recent clinical studies of transcutaneous electrical nerve stimulation on xerostomia – pubmed and domestic studies. J Int Korean Med 2022;43(3):375-86. https://doi.org/10.22246/jikm.2022.43.3.375
[DOI]
18. Joung SA. Effects of normal saline solution mouthwash on oral health status, xerostomia, Halitosis and salivary pH in elders in long-term care facilities. J Korean Gerontol Nurs 2017;19(3):173-83. https://doi.org/10.17079/jkgn.2017.19.3.173
[DOI]
19. Kim YS, Shin KH, Park JR, Chung SH, Choi HS. The effect of oral function improvement with oral exercise program by elderly people. J Korean Soc Dent Hyg 2016;16(4):559-66. https://doi.org/10.13065/jksdh.2016.16.04.559
[DOI]
20. Park JH, Sohng KY. Comparison of oral care interventions on oral status for intubated intensive care unit patients. J Korean Acad Fundam Nurs 2010;17(3):324-33.
21. Munro CL, Grap MJ, Jones DJ, McClish DK, Sessler CN. Chlorhexadine, toothbrushing and preventing vetilator ssociated pneumonia in critically ill adults. Am J Crit Care 2009;18(5):428-37. https://doi.org/10.4037/ajcc2009792
[DOI][PubMed][PMC]
22. Jeon YJ, Choi JS, Han SJ. The effect of dry mouth improvement by oral exercise program in elderly people. J Korean Soc Dent Hyg 2012;12(2):293-305. https://doi.org/10.13065/jksdh.2012.12.2.293
[DOI]
23. Jang KA, Kim GE, Heo SE. The effect of professional oral care by time point on oral health status of inpatients in a nursing hospital. J Korean Society of Oral Health Science 2019;7(3):92-7. https://doi.org/10.33615/jkohs.2019.7.3.92
[DOI]