Introduction
Frailty is defined as a state of physical weakness characterized by a marked decline in the functions of various organs and systems, resulting in reduced resilience or resistance to external stress. The number of older adults in Korea was approximately 410,053 in 2008; however, this number is projected to reach 1,197,697 by 2030 and 2,051,153 by 2050. The pre-frail population comprised 2,453,387 individuals in 2008, and this number is projected to reach 1,068,815 in 2050. This increase is expected to be accompanied by an increase in medical costs. Frailty represents an intermediate stage between health and disability; thus, returning to a healthy state with or without individual effort may be possible, and prevention and management are of utmost importance [1].
Oral frailty, an early symptom of generalized physical frailty, is an age-related condition characterized by a decrease in oral and maxillofacial function, a decrease in physiologic function, and poor oral hygiene [2,3]. A systematic review of factors related to oral frailty among older adults revealed that among the 12 oral health indicators related to frailty, the number of teeth present, decrease in masticatory function, difficulty in chewing, deterioration of oral health, oral diadochokinesis, and decrease in bite force showed strong associations with frailty. In particular, loss of multiple teeth and poor oral health were identified as factors that showed the strongest associations with frailty [4]. In Korea, oral frailty is diagnosed among individuals aged ≥65 years based on impairment in at least two of the following items: masticatory function, occlusal force, tongue muscle strength, salivary gland function (xerostomia), swallowing function, and oral hygiene maintenance status [3].
Oral frailty is a risk factor for the incidence of frailty during the pre-frailty stage. Oral frailty increases the risk of physical frailty, sarcopenia, disability, and mortality among older adults. Notably, poor oral health status has been identified as a risk factor for frailty [5,6]. The number of remaining teeth, masticatory function, cumulative oral health problems, and xerostomia affect the onset of frailty and can be used as predictors of the incidence of frailty during old age [7]. Eating alone has shown a strong association with the incidence of oral frailty; oral health is also associated with social life and social isolation among older adults [8,9]. Diagnosing and implementing interventions for oral frailty can restore oral function, prevent systemic frailty, and improve the quality of life (QOL) in older adults [10]. Chewing difficulty, speech difficulty due to dry mouth or decreased tongue strength, loss of multiple teeth, and poor oral hygiene are predictors of oral frailty.
The eight-item Health-related Quality of Life Instrument (HINT-8) was introduced in the first year of the eighth Korean National Health and Nutrition Examination Survey (KNHANES) to facilitate more precise measurement of the health-related QOL (HRQOL) in Korea. HINT-8 is divided into four health domains: physical health (climbing stairs, pain, and vitality), social health (work), mental health (depression, memory, and sleep), and positive health (happiness) domains. The instrument comprises eight items designed to express the health status with the preceding week as the recall period [11].
A previous study examining the effects of the number of days of walking on the HINT-8 score and oral health behaviors on individuals aged 19–69 years revealed that the number of days of walking was associated with the HINT-8 score and oral health behaviors. Another study reported that oral health promotion and treatment had a significant effect on the HINT-8 score among individuals aged ≥19 years [12,13]. The presence of a greater number of intraoral prostheses was associated with difficulty in climbing stairs, pain, and memory among individuals aged 40–64 years in a previous study [14]. Another study on women aged 30–69 years revealed that grip strength affected the oral health and dental care needs, the requirement for dental care, and QOL [15]. A study on middle-aged women aged 40–64 years revealed that economic status had a positive effect on QOL and that this effect may be reduced by oral health status [16]. Although several recent studies on oral health have used HINT-8, studies related to oral frailty that used HINT-8 remain lacking. Oral frailty is expected to have a major impact on future medical expenditures owing to the increase in the number of older adults. Moreover, it is a risk factor for systemic frailty. Thus, the prevention, early diagnosis, and management of oral frailty can improve the oral health status of older adults, reduce medical expenditure, improve systemic health, and improve QOL. This study aimed to identify the prevalence of oral frailty in older adults and the association between oral frailty and the HINT-8 score. The findings of the present study can be used as basic data for formulating future policies on the management of oral frailty and will contribute to the improvement of HRQOL by improving the oral health status of this population.
Methods
1. Participants
Secondary analysis was performed using the raw data from the 2019 KNHANES, the eighth round of which included oral examinations. The study population comprised 1,318 adults aged ≥65 years. The sex, age, income quartile (household), education level, chewing discomfort, speech difficulty, number of remaining natural teeth, brushing frequency, and use of oral hygiene products were recorded. KNHANES qualifies as a study conducted directly by the government for public welfare according to Article 2 (1) of the Bioethics Act and Article 2 (2) (1) of the Enforcement Rules of the same Act. Therefore, Institutional Review Board (IRB) approval was not required. Nevertheless, IRB approval (2018-01-03-3C-A) was obtained in consideration of the collection of human-derived materials and the provision of raw data to third parties.
2. Instrument
The following variables were analyzed in this study to investigate the association between oral frailty and the HINT-8 score:
(1) General characteristics
Data regarding the general characteristics of the study population, including sex, age, income quartile (household), and education level, were recorded during the survey. The income quartiles (household) were divided into ‘high,’ ‘high-middle,’ ‘low-middle,’ and ‘low.’ Education level was divided into ‘≤primary school,’ ‘middle school,’ ‘high school,’ and ‘≥college.’
(2) Oral frailty
Previous studies have identified chewing difficulty, speech difficulty due to dry mouth or reduced tongue strength, loss of multiple teeth, and poor oral hygiene status as predictors of oral frailty. Therefore, the five items of oral frailty were defined in this study using the items surveyed in KNHANES. ‘Chewing discomfort’ was used as a substitute for masticatory function, ‘number of natural teeth present’ for occlusal force, ‘speech difficulty’ for dry mouth and tongue strength, and ‘frequency of brushing’ and ‘use of oral hygiene products’ for oral hygiene status. Impairment of one or more of the aforementioned items indicated oral frailty. The responses of ‘very uncomfortable’ and ‘uncomfortable’ for ‘speech difficulty’ indicated oral frailty. The presence of ≤19 natural teeth was considered to indicate oral frailty in accordance with the expert consensus on the Diagnostic criteria and treatment of oral senility in Korea [3]. The oral hygiene status was determined based on ‘brushing frequency’ and ‘use of oral hygiene products.’ Brushing frequency was divided into the following categories: ‘before and after breakfast,’ ‘before and after lunch,’ ‘before and after dinner,’ ‘after snacks,’ and ‘before bedtime.’ The average brushing frequency was calculated based on the total number of times the individual brushed their teeth. The oral hygiene products used included ‘floss,’ ‘interdental brush,’ ‘mouthwash,’ ‘electric toothbrush,’ and ‘others.’ The frequency of using these products was summed. Brushing frequency and use of oral hygiene products are indicators of oral hygiene status. Poor oral hygiene status was defined as less than the average of brushing frequency and use of oral hygiene products. The average brushing frequency and frequency of using oral hygiene products for individuals aged ≥65 years were calculated (2.46 and 0.59, respectively). A brushing frequency below the average (twice daily) and not using oral hygiene products indicated oral frailty.
(3) HINT-8
The eight items of the HINT-8 (climbing stairs, pain, vitality, work, depression, memory, sleep, and happiness) and four health domains (physical health, social health, mental health, and positive health domains) were analyzed in this study. The physical health domain comprises climbing stairs, pain, and vitality; the social health domain comprises working; the mental health domain comprises depression, memory, and sleep; and the positive health domain comprises happiness [11]. Higher scores for each of these items indicated lower HRQOL.
3. Data analysis
Complex sample statistical analyses were performed using variance estimation strata (kstrata), survey unit (psu), and oral examination weight (wt_oe) to ensure that the results of the analysis were representative. Continuous and categorical variables are presented as mean±standard error and frequency (weighted percentage), respectively. The general characteristics of the participants were analyzed via complex sample cross-analysis and generalized linear model analysis according to the oral frailty status. The association between oral frailty and the HINT-8 score was analyzed using complex sample logistic regression analysis. The association between oral frailty and the HINT-8 score after adjusting for general characteristics was analyzed using complex sample multiple logistic regression analysis. All statistical analyses were performed using IBM SPSS Statistics (version 23.0; IBM Corp., Armonk, NY, USA), The significance level was set to α=0.05.
Results
1. General characteristics of the participants according to the oral frailty status
(Table 1) presents the general characteristics of the participants according to the oral frailty status. Chewing difficulty, speech difficulty, number of remaining teeth, and brushing frequency showed statistically significant associations with age, income level, and education level. The use of oral hygiene products showed statistically significant associations with sex, age, and education level. The mean age of the participants with chewing and speech difficulties was 73.55 and 73.93 years, respectively. These difficulties were observed at a higher rate among those with lower income and education levels. The mean age of individuals with ≤19 remaining teeth was 74.31 years. The proportion of individuals with ≥20 remaining teeth was higher among those with higher income and education levels. The mean age of individuals who brushed ≤2 times per day was 73.07 years. The proportion of individuals who brushed ≥3 times per day was higher among those with higher income and education levels. Women were more likely to use oral hygiene products than men. The mean age of individuals who used oral hygiene products was 71.74 years. The proportion of individuals using oral hygiene products was higher among those with higher education levels (p<0.05).
2. Association between oral frailty and the HINT-8 items
(Table 2) presents the association between oral frailty and the HINT-8 items. Compared with that among those without chewing difficulty, the prevalence of difficulty in climbing stairs, pain, difficulty in working, difficulty in remembering, and being unhappy was 1.573, 1.263, 1.323, 1.461, and 1.202 times higher, respectively, among individuals with chewing difficulty. In contrast, the prevalence of depression was 0.833 times lower among individuals with chewing difficulty (p<0.05). Compared with that among those without speech difficulty, the prevalence of difficulty in climbing stairs, difficulty in working, and difficulty in remembering was 1.582, 1.421, and 1.700 times higher, respectively, among individuals with speech difficulty (p<0.05). Compared with that among individuals with ≥20 remaining teeth, the prevalence of difficulty in climbing stairs, difficulty in working, difficulty in remembering, and being unhappy was 2.124, 1.508, 1.422, and 1.182 times higher, respectively, among individuals with ≤19 remaining teeth; in contrast, the prevalence of depression was 0.594 lower (p<0.05). Compared with that among those with an average brushing frequency of ≥3, the prevalence of difficulty in climbing stairs, difficulty in remembering, and being unhappy was 1.253, 1.130, and 1.174 times higher, respectively, among individuals with an average brushing frequency of ≤2; in contrast, the prevalence of depression was 0.869 times lower (p<0.05). Compared with that among those who use oral hygiene products, the prevalence of difficulty in climbing stairs, difficulty in working, and difficulty in remembering was 1.168, 1.235, and 1.166 times higher, respectively, among individuals who do not use oral hygiene products; in contrast, the prevalence of pain and depression was 0.870 and 0.724 times lower, respectively (p<0.05).
The overall HINT-8 scores were 1.183, 1.236, 1.153, and 1.043 times lower among individuals with chewing difficulty, speech difficulty, ≤19 remaining teeth, and average brushing frequency of ≤2 times, respectively, compared with those of their counterparts (p<0.05).
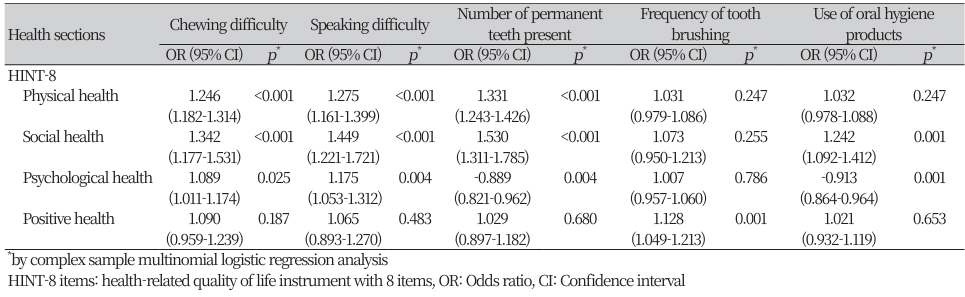
3. Association between oral frailty and the health domain of HINT-8
(Table 3) presents the association between oral frailty and the health domain of HINT-8. The QOL of individuals with chewing difficulty in the domains of physical health, social health, and mental health was 1.246, 1.324, and 1.089 times lower, respectively, than that of those without chewing difficulty (p<0.05). The QOL of individuals with speech difficulty in the domains of physical health, social health, and mental health domains was 1.275, 1.449, and 1.175 times lower, respectively, than that of those without speech difficulty (p<0.05). The QOL of individuals with ≤19 remaining teeth in the domains of physical health and social health was 1.331 and 1.530 times lower, respectively, than that of those individuals with ≥20 remaining teeth; in contrast, the QOL in the mental health domain was 0.889 times higher (p<0.05). The QOL of individuals with an average brushing frequency of ≥2 in the positive health domain was 1.128 times lower than that among individuals with an average brushing frequency of ≥3 times (p<0.05). The QOL of individuals who did not use oral hygiene products in the social health domain was 1.242 times lower than that of those who used oral hygiene products; in contrast, the QOL in the social health domain was 0.913 times higher (p<0.05).
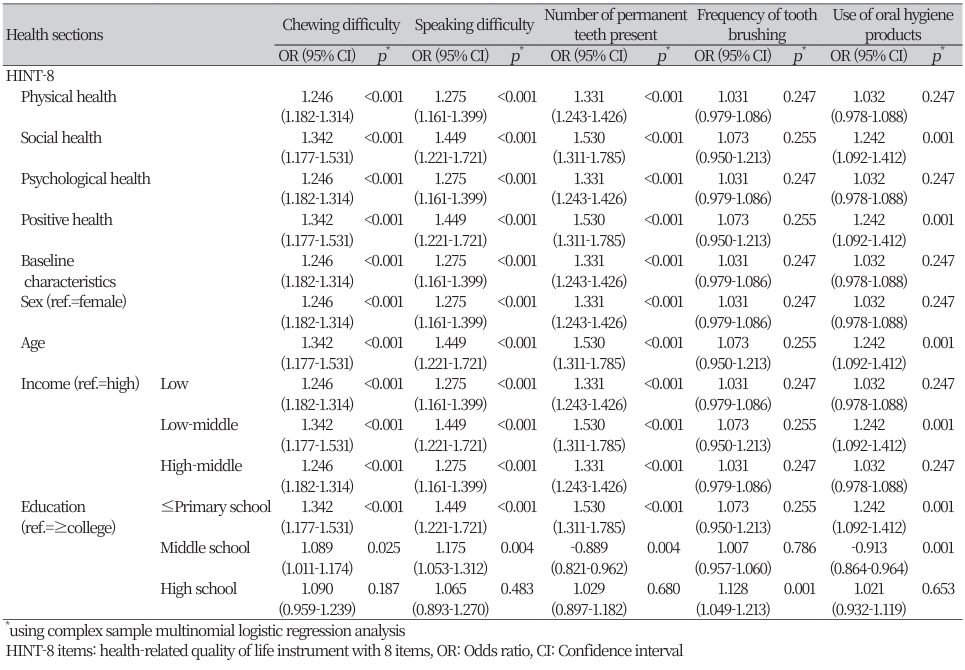
(Table 4) presents the association between oral frailty and the health domain of HINT-8 adjusted for the general characteristics of the participants. The QOL of individuals with chewing difficulty in the domains of physical health and mental health and QOL of individuals with speech difficulty in the domains of physical health, social health, and mental health showed statistically significant differences. The QOL of individuals with ≤19 remaining teeth in the physical health domain, QOL of individuals with an average brushing frequency of ≤2 in the positive health domain, and QOL of individuals who use oral hygiene products in the mental health domain showed significant differences (p<0.05).
Discussion
A poor oral environment can lead to poor oral and dental health. Poor oral health status leads to poor nutrition owing to the inability to Meat, which in turn leads to systemic frailty. Thus, oral health acts as a risk factor for developing systemic frailty.
Chewing difficulty, speech difficulty, ≤19 natural teeth, and poor oral hygiene status (brushing frequency of ≤2 times per day and not using oral hygiene products) were observed in older adults with oral frailty in the present study. Notably, 34.6%, 13.8%, 39.1%, and 55% of older adults aged ≥65 years had chewing difficulty, speech difficulty, ≤19 remaining teeth, and brushing frequency of ≤2 times per day, respectively; moreover, 53.4% did not use oral hygiene products (data not shown in the tables). These results indicate that more than half of older adults in Korea have poor oral health, approximately 40% have few remaining teeth, approximately 35% experience chewing discomfort, and approximately 55% experience symptoms of oral frailty. A recent systematic review on oral frailty revealed that the 12 oral health indicators associated with frailty in older adults aged ≥60 years could be classified into four categories. Moreover, deterioration of oral health status (number of remaining teeth, oral health, periodontal disease, and oral dysbiosis) was observed in 52% of older adults; deterioration of oral motor function (occlusal force, tongue pressure, masticatory function, and oral diadochokinesis) in 27%; chewing, swallowing, and salivary disorders (dry mouth, chewing difficulty, and swallowing difficulty) in 20%; and oral pain (tooth or mouth pain) in 1%. Among the 12 oral health indicators associated with frailty, the number of remaining teeth (29%), poor oral health status (15%), chewing difficulty (11%), reduced masticatory function (9%), reduced occlusal force (7%), and oral diadochokinesis (5%) showed strong associations with frailty. In particular, the presence of fewer natural teeth and poor oral health status were identified as the predictors most frequently associated with frailty, which was consistent with the findings of the present study [4].
Oral frailty showed associations with age, income level, and education level. A mean age of ≥73 years was associated with a higher prevalence of chewing difficulty, speech difficulty, brushing frequency of ≤2 times per day, and not using oral hygiene products. A mean age of ≥74 years was associated with a higher prevalence of the presence of ≤19 remaining teeth. These findings also confirmed that oral frailty was more common among individuals with lower income and education levels. Park and Kim [17] used raw data from the first year of the sixth KNHANES to evaluate the status of oral hygiene care among older adults aged ≥65 years and revealed that the brushing frequency of individuals with lower education levels was lower than that of those with higher education level and that those with lower education level and household income used fewer oral hygiene products. In addition, older adults with chewing and masticatory difficulties used fewer oral hygiene products than their counterparts. Ju et al. [18] used raw data from the first and second years of the seventh KNHANES to evaluate the oral health problems observed in older adults aged ≥65 years and revealed that the prevalence of chewing and speech difficulties was higher among individuals with lower household income and education levels than their counterparts, which is consistent with the finding of the present study. Thus, these findings confirm that the symptoms of oral frailty are closely associated with the income and education levels, indicating that individuals with low income and education levels are more likely to experience chewing and speech difficulties and have a poorer oral hygiene status compared with their counterparts. Thus, policy measures, such as improving health insurance and expanding insurance coverage for dentures and implants, should be established to prioritize the creation of oral hygiene care groups for individuals with low income and education levels and to resolve chewing and speech difficulties to reduce oral frailty in older adults.
Comparison between chewing difficulty and the health domains of HINT-8 revealed that individuals with chewing difficulty had lower QOL in the domains of physical health, social health, and mental health compared with that of those without chewing difficulty (p<0.05). Ju et al. [18] analyzed the effects of HRQOL (EQ-5D) on chewing difficulty in older adults and revealed that chewing difficulty increased by 1.849, 1.790, and 1.677 times in the groups with no exercise capacity, pain and discomfort, and anxiety and depression, respectively. In addition, analysis of the effects of HRQOL (EQ-5D) on speech difficulty in older adults revealed that speech difficulty increased by 2.385, 1.693, and 2.111 times in the group with no exercise capacity, pain and discomfort, and anxiety and depression, respectively. Kim et al. [19] used raw data from the first year of the eighth KNHANES to evaluate the effects on QOL and oral health status among older adults aged ≥65 years and revealed that chewing and speech difficulties were associated with a lower HRQOL assessed by EQ-5D and HINT-8. Direct comparisons may be difficult owing to the use of different HRQOL instruments in the present and previous studies; however, all studies demonstrated that chewing and speech difficulties were closely associated with poor HRQOL. Thus, symptoms of oral frailty, such as chewing and speech difficulties, must be prevented and treated to improve the HRQOL of older adults. Persistent chewing difficulty can be fatal to older adults, as it can limit nutritional intake and cause deterioration of systemic health. In contrast, speech difficulty can interfere with their interpersonal and social activities, leading to social isolation. Therefore, older adults must be provided active social and financial support to restore their oral function, which in turn can improve their basic QOL, prevent social isolation, and improve mental health.
Comparison between the number of remaining teeth and health domains of HINT-8 revealed that individuals with ≤19 teeth had lower QOL in the domains of physical health and social health compared with that of those with ≥20 teeth (p<0.05). Comparison between the number of remaining teeth and the items of HINT-8 revealed that individuals with ≤19 teeth experienced greater difficulty in climbing stairs, greater difficulty in working, greater difficulty in remembering, and less happiness than individuals with ≥20 teeth (p<0.05). A systematic review of QOL and the number of teeth in older adults conducted by Lee et al. [20] revealed that the QOL of individuals with at least one tooth remaining was higher than that of edentulous individuals, the QOL decreased significantly when the number of remaining teeth was ≤9, and the QOL scores were higher when the number of remaining teeth was ≥20. Their study also revealed that the physical index, one of the measures of QOL, was lower in individuals with fewer teeth and that QOL decreased significantly with the loss of anterior teeth. These findings confirmed that the number of remaining teeth has a very important effect on QOL in older adults. Tooth loss may occur due to various causes, including dental caries, periodontal disease, and trauma, and the remnants may be retained even after treatment. Thus, oral health care system for the entire lifespan, starting from deciduous teeth to permanent teeth, is required. Furthermore, systematic oral health care must also be implemented.
Comparison between brushing frequency and the health domains of the HINT-8 revealed that individuals with an average brushing frequency of ≤2 times per day had lower QOL in the positive health domain than those with an average brushing frequency of ≥3 times per day (p<0.05). Comparison between the use of oral hygiene products and the health domains of HINT-8 revealed that individuals who did not use oral hygiene products had lower QOL in the social health domain compared with that of those who did (p<0.05). Kim et al. [19] also reported that not brushing teeth the preceding day was associated with lower HRQOL assessed by EQ-5D and HINT-8. Brushing and the use of oral hygiene products play essential roles in maintaining oral health. Poor oral hygiene can lead to poor oral health status and tooth loss, which can lead to unbalanced dietary intake that can cause systemic frailty. Thus, it is important to manage oral frailty as poor oral hygiene can lead to oral frailty and systemic frailty. The QOL of older adults will improve if oral frailty can be prevented via early diagnosis and active interventions, leading to a healthy life in the future. Thus, it is necessary to raise awareness regarding the importance of oral health among older adults and develop specialized programs for the management and prevention of oral frailty, in addition to establishing policy-based systems.
This study has some limitations. First, among the various symptoms of oral frailty, only masticatory function, occlusal force, tongue strength, and oral hygiene were assessed using items from the KNHANES data in the present study. However, this study is significant in that it is the first study to investigate the association between oral frailty and HRQOL in older adults aged ≥65 years using national survey data with proven reliability and validity. Future studies should investigate oral frailty among older adults using the recently developed diagnostic criteria for the treatment of oral frailty in Korea. Such efforts should be supported by policy-based discussions to systematically manage oral frailty.
Conclusions
This study used data from the first year of the eighth KNHANES to investigate the association between oral frailty and HINT-8 among older adults aged ≥65 years and aimed to use the findings as basic data for establishing policies related to the management of oral frailty among older adults. The conclusions derived from the study were as follows:
1. HINT-8 was 1.183, 1.236, 1.153, and 1.043 times lower among individuals with chewing difficulty, speech difficulty, ≤19 remaining teeth, and brushing frequency of ≤2 times per day, respectively (p<0.05).
2. The QOL in the domains of physical health, social health, and mental health was 1.246, 1.324, and 1.089 times lower, respectively, among individuals with chewing difficulty (p<0.05).
3. The QOL in the domains of physical health, social health, and mental health was 1.275, 1.449, and 1.175 times lower, respectively, among individuals with speech difficulty (p<0.05).
4. The QOL in the domains of physical health and social health was 1.331 and 1.530 times lower, respectively, among individuals with ≤19 remaining teeth; in contrast, the QOL in the mental health domain was 0.889 times higher (p<0.05).
5. The QOL in the positive health domain was 1.128 times lower among individuals with an average brushing frequency of ≤2 times per day. The QOL in the social health domain was 1.242 times lower in individuals who did not use oral hygiene products; in contrast, the QOL in the mental health domain was 0.913 times higher (p<0.05).
The present study demonstrated that oral frailty caused a decline in HRQOL among older adults and that approximately 55% of older adults experience symptoms of oral frailty. These findings suggest the requirement for developing policies related to the management of oral frailty among older adults and implementing specialized programs for the management of oral frailty.
Notes
Author Contributions
Conceptualization: SJ Sim, SM Lee; Data collection: SJ Sim; Formal analysis: SJ Sim, SM Lee; Writing-original draft: SJ Sim, SM Lee; Writing-review&editing: SJ Sim, SM Lee
Conflicts of Interest
The authors declared no conflicts of interest.
Funding
None.
Ethical Statement
This study was approved by the Institutional Review Board of Baekseok University (BUIRB-202304-HR-006).
Acknowledgements
None.